一项回顾性队列研究:血尿素氮引导蛋白剂量调整有助于减少神经危重症患者高蛋白摄入导致的氮血症和功能预后恶化
IF 3.1
3区 医学
Q2 NUTRITION & DIETETICS
引用次数: 0
摘要
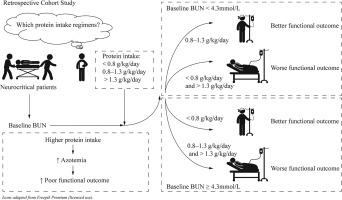
神经危重症患者的最佳蛋白质剂量仍不确定。我们假设较高的蛋白质剂量增加氮血症风险并恶化预后,基线BUN可以指导蛋白质剂量的调整。在这项单中心、回顾性队列研究中,我们纳入了2018年7月至2023年6月期间入院的327名18岁及以上的神经危重症患者(BMI: 18.5-30 kg/m2)。计算了所有来源的每日蛋白质摄入量。主要终点为氮血症发生率,次要终点为30天功能预后(mRS >3)。根据蛋白质摄入量对患者进行分类:0.8 g/kg/d、0.8 ~ 1.3 g/kg/d和1.3 g/kg/d。与1.3 g/kg/d组相比,0.8 g/kg/d组氮血症发生率较低(21.9% vs. 45.7%,校正p = 0.002),校正混杂因素后相关性显著。在APACHE II评分为15分的患者中,0.8 g/kg/d组氮血症发生率较低,预后较好。对于评分≥15的患者,1.3 g/kg/d组氮血症发生率较高,预后较差。0.8 g/kg/d组BUN与30天预后呈u型关系。对于BUN < 4.3 mmol/L,蛋白质摄入0.8 - 1.3 g/kg/d改善结果,而对于BUN < 4.3 mmol/L,蛋白质摄入0.8 g/kg/d有益。研究表明,过量的蛋白质摄入与氮血症风险增加和更糟糕的结果有关。基线BUN可能有助于神经危重症护理中蛋白质剂量的选择,尽管其普遍性需要在多中心前瞻性研究中验证。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Blood urea nitrogen-guided protein dosage adjustment helps reduce azotemia and functional prognosis deterioration induced by high protein intake in neurocritical patients: A retrospective cohort study
The optimal protein dosage for neurocritical patients remains uncertain. We hypothesized that higher protein dosage increases azotemia risk and worsens prognosis, and that baseline BUN can guide protein dosage adjustments. In this single-center, retrospective cohort study, we included 327 neurocritical patients aged 18 or older admitted between July 2018 and June 2023 (BMI: 18.5-30 kg/m2). Daily protein intake from all sources was calculated. The primary outcome was azotemia incidence, and secondary outcomes included 30-day functional prognosis (mRS >3). Patients were categorized by protein intake: <0.8 g/kg/d, 0.8–1.3 g/kg/d, and >1.3 g/kg/d. Azotemia incidence was lower in the <0.8 g/kg/d group compared to the >1.3 g/kg/d group (21.9 vs. 45.7%, adjusted p = 0.002), with a significant correlation after adjusting for confounders. Among patients with an APACHE II score <15, the <0.8 g/kg/d group had lower azotemia rates and better prognosis. For those with a score ≥15, the >1.3 g/kg/d group had higher azotemia rates and worse prognosis. A U-shaped relationship between BUN and 30-day prognosis was observed in the <0.8 g/kg/d group. For BUN <4.3 mmol/L, protein intake of 0.8–1.3 g/kg/d improved outcomes, whereas for BUN >4.3 mmol/L, intake <0.8 g/kg/d was beneficial. The research demonstrates that excessive protein intake is associated with increased azotemia risk and worse outcomes. Baseline BUN may help inform protein dosage selection in neurocritical care, though its generalizability requires validation in multicenter prospective studies.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Nutrition Research
医学-营养学
CiteScore
7.60
自引率
2.20%
发文量
107
审稿时长
58 days
期刊介绍:
Nutrition Research publishes original research articles, communications, and reviews on basic and applied nutrition. The mission of Nutrition Research is to serve as the journal for global communication of nutrition and life sciences research on diet and health. The field of nutrition sciences includes, but is not limited to, the study of nutrients during growth, reproduction, aging, health, and disease.
Articles covering basic and applied research on all aspects of nutrition sciences are encouraged, including: nutritional biochemistry and metabolism; metabolomics, nutrient gene interactions; nutrient requirements for health; nutrition and disease; digestion and absorption; nutritional anthropology; epidemiology; the influence of socioeconomic and cultural factors on nutrition of the individual and the community; the impact of nutrient intake on disease response and behavior; the consequences of nutritional deficiency on growth and development, endocrine and nervous systems, and immunity; nutrition and gut microbiota; food intolerance and allergy; nutrient drug interactions; nutrition and aging; nutrition and cancer; obesity; diabetes; and intervention programs.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


