抗精神病药物引起的镇静不良事件的发展轨迹:一项对急性期精神分裂症随机、安慰剂对照临床试验个体参与者数据的荟萃分析
IF 30.8
1区 医学
Q1 PSYCHIATRY
引用次数: 0
摘要
背景镇静不良事件在精神分裂症患者接受抗精神病药物治疗中很常见,影响治疗依从性和患者的生活质量。虽然对镇静的耐受性被认为是发展的,但记录镇静开始和消退时间的有力证据仍然难以捉摸。为了解决这一差距,我们旨在评估精神分裂症患者中各种抗精神病药物镇静起效和消退的动态。方法在这项荟萃分析中,我们纳入了抗精神病单药治疗急性期精神分裂症和分裂情感性障碍的安慰剂对照、随机对照试验(RCTs)。我们在PubMed检索了从开始到2021年5月6日的随机对照试验,并通过耶鲁大学开放数据获取项目获得了纳入试验的个体参与者数据。我们创建Kaplan-Meier曲线来评估镇静发生的概率和治疗开始后镇静发生率随时间的消退。有生活经验的人没有参与这项研究。本研究已注册为PROSPERO, CRD42022351647。结果:我们共纳入了来自19项随机对照试验的6791名参与者(男性4549名[67.0%],女性2242名[33.0%],平均年龄为38.0岁[SD 12.4,范围13-81],亚洲人1172名[17.3%],黑人1626名[23.9%],白人3654名[53.8%],其他种族339名[5.0%])。6791名参与者中有582人(8.6%)出现镇静不良事件,通常发生在治疗开始后不久。在接受抗精神病药物治疗的参与者中,505例镇静事件中有418例(83%)发生在治疗的前2周。镇静开始后,50%的症状在1周内消失。治疗4周后,24% (95% CI 19.7 ~ 29.3)的患者继续使用口服药物镇静,22.3%(15.3 ~ 32.3)的患者继续使用长效注射剂镇静。抗精神病药物治疗的前2周内镇静的高发生率强调了早期监测的重要性。半数镇静在1周内消退,75%在1个月内消退,提示镇静耐受性获得迅速。如果镇静持续,应评估影响因素。资助德国联邦教育和研究部。本文章由计算机程序翻译,如有差异,请以英文原文为准。
The trajectory of sedative adverse events caused by antipsychotics: a meta-analysis of individual participant data from randomised, placebo-controlled, clinical trials in acute phase schizophrenia
Background
Sedative adverse events are common in patients with schizophrenia undergoing antipsychotic treatment, which affects treatment adherence and the patients’ quality of life. Although tolerance to sedation is believed to develop, robust evidence documenting the timing of sedation onset and resolution remains elusive. To address this gap, we aimed to assess the dynamics of onset and resolution of sedation across various antipsychotics in patients with schizophrenia.Methods
In this meta-analysis, we included placebo-controlled, randomised controlled trials (RCTs) of antipsychotic monotherapy for the acute phase of schizophrenia and schizoaffective disorder. We searched PubMed for RCTs from inception until May 6, 2021 and obtained individual participant data of included trials through the Yale University Open Data Access project. We created Kaplan–Meier curves to assess the probability of onset of sedation and resolution from the incidence of sedation across time after treatment initiation. People with lived experience were not involved in this study. This study is registered with PROSPERO, CRD42022351647.Findings
We included a total of 6791 participants (4549 [67·0%] men and 2242 [33·0%] women, with a mean age of 38·0 years [SD 12·4, range 13–81], 1172 [17·3%] were Asian, 1626 [23·9%] were Black, 3654 [53·8%] were White, and 339 [5·0%] were other ethnicities) from 19 RCTs. Sedative adverse events were observed in 582 (8·6%) of 6791 participants and typically occurred shortly after treatment initiation. Among participants receiving antipsychotics, 418 (83%) of 505 sedation events occurred within the first 2 weeks of treatment. Following the onset of sedation, 50% of symptoms were resolved within 1 week. After 4 weeks of treatment, 24% (95% CI 19·7–29·3) continued to have sedation with oral agents and 22·3% (15·3–32·3) with long-acting injectables.Interpretation
The high incidence of sedation within the first 2 weeks of treatment with antipsychotics emphasises the importance of early monitoring. Half of the sedation resolved within 1 week and 75% within 1 month, suggesting that tolerance to sedation is acquired quickly. If sedation is sustained, contributing factors should be evaluated.Funding
German Federal Ministry of Education and Research.求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
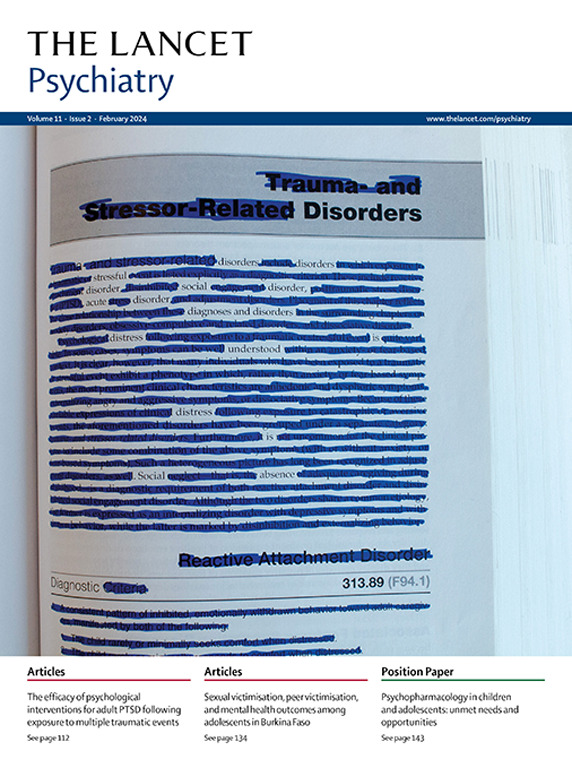
Lancet Psychiatry
PSYCHIATRY-
CiteScore
58.30
自引率
0.90%
发文量
0
期刊介绍:
The Lancet Psychiatry is a globally renowned and trusted resource for groundbreaking research in the field of psychiatry. We specialize in publishing original studies that contribute to transforming and shedding light on important aspects of psychiatric practice. Our comprehensive coverage extends to diverse topics including psychopharmacology, psychotherapy, and psychosocial approaches that address psychiatric disorders throughout the lifespan. We aim to channel innovative treatments and examine the biological research that forms the foundation of such advancements. Our journal also explores novel service delivery methods and promotes fresh perspectives on mental illness, emphasizing the significant contributions of social psychiatry.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


