实施第一版巴黎报告制度的影响:系统回顾和荟萃分析。
摘要
尿液细胞学是一种非侵入性的诊断工具,广泛用于筛查和监测泌尿生殖道肿瘤。然而,由于缺乏统一的术语和明确的客观形态学标准,限制了尿液细胞学的临床应用。巴黎尿液细胞学报告系统(TPS)的开发旨在规范尿液细胞学报告,提高尿液细胞学检测高级别恶性肿瘤(HGM)的性能。我们旨在通过进行系统回顾和荟萃分析,评估 TPS 对提高尿液细胞学诊断效果和临床实用性的潜在影响。我们检索了六个电子数据库,以确定从 2004 年 1 月到 2022 年 12 月期间评估尿液细胞学在检测受监控或临床怀疑为恶性肿瘤的患者的泌尿生殖道恶性肿瘤方面的准确性的英文横断面和队列研究。我们从符合条件的研究中提取了相关数据,以计算细胞学诊断类别的相对分布;非典型细胞学诊断与 HGM 细胞学诊断的比率;以及与细胞学诊断类别相关的 HGM 风险 (ROHGM) 和 HGM 可能性比 (HGM-LR)。我们使用了带有 logit 变换的广义线性混合模型来组合比例,并使用多层次混合效应逻辑回归来汇集诊断准确性测量结果。我们进行了元回归,以评估 TPS 和非 TPS 队列之间的显著差异。我们共纳入了 64 项研究,涉及 31 个 TPS 和 49 个非 TPS 队列中的 99,796 份合并细胞学样本。在满意的细胞学病例中,高级别尿路上皮癌阴性(NHGUC)/恶性肿瘤阴性(NM)、非典型尿路上皮细胞(AUC)、高级别尿路上皮癌可疑(SHGUC)/恶性肿瘤可疑(SM)、低级别尿路上皮肿瘤(LGUN)和HGM类别的汇总相对分布[95%置信区间(CI)]为83.8%(80.3%-86.9%)、8.0%(6.0%-10.6%)、2.2%(1.4%-3.3%)、0.01%(0.0%-0.1%)和4.2%(3.2%-5.5%)。8%(76.8%-2.7%)、11.3%(8.6%-14.7%)、1.8%(1.2%-2.7%)、0.01%(0.0%-0.1%)和 3.3%(2.5%-4.3%)。采用 TPS 分类后,NHGUC 和 AUC 细胞学诊断的频率分别显著增加和减少。TPS队列中的AUC/HGM比率为2.0,与非TPS队列中的非典型/HGM比率4.1相比,差异有统计学意义(P值:0.01)。此外,与非 TPS 队列中的 34.1%(26.4%-42.8%)相比,TPS 队列中 LGUN 在细胞学上称为 AUC 的汇总率(95% CI)显著下降至 20.8%(14.9%-28.3%)。在 TPS 研究中,汇总的 ROHGM(95% CI)在非诊断 (NDX) 中为 20.4% (6.2%-50.0%),在 NHGUC 中为 15.5% (9.6%-24.2%),在 AUC 中为 40.2% (30.9%-50.2%),在 SHGUC 中为 80.8% (72.9%-86.8%),在 LGUN 中为 15.1% (5.7%-34.3%),在 HGM 类别中为 91.4% (87.3%-94.3%)。NHGUC、AUC、SHGUC 和 HGM 类别与 HGM-LR 的相关性(95% CI)分别为 0.2(0.1-0.3)、0.9(0.6-1.3)、6.9(2.4-19.9)和 16.8(8.3-33.8)。我们的结果表明,TPS 1.0 降低了 AUC 诊断的相对频率、AUC/HGM 比率以及细胞学诊断为 AUC 的 LGUN 的频率。采用这种分类提高了 SHGUC 和 HGM 细胞学诊断在判定高级别病变时的临床实用性。然而,NHGUC 诊断并不能可靠地排除高级别病变的存在。
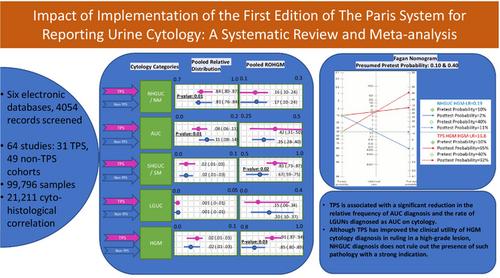
Urine cytology is a noninvasive, widely used diagnostic tool for screening and surveillance of genitourinary tract neoplasms. However, the absence of unified terminology and clear objective morphological criteria limits the clinical benefit of urine cytology. The Paris System for Reporting Urine Cytology (TPS) was developed with the goal of standardizing reporting and improving urine cytology performance in detecting high-grade malignancy (HGM). We aimed to evaluate potential effects of TPS on improving urine cytology diagnostic performance and clinical utility by conducting a systematic review and meta-analysis. We searched six electronic databases to identify cross-sectional and cohort studies written in English assessing the accuracy of urine cytology in detecting genitourinary tract malignancies of patients under surveillance or with clinical suspicion of malignancy from January 2004 to December 2022. We extracted relevant data from eligible studies to calculate relative distribution of cytology diagnostic categories; ratio of atypical to HGM cytology diagnosis; and risk of HGM (ROHGM) and HGM likelihood ratio (HGM-LR) associated with cytology diagnostic categories. We used a generalized linear mixed model with logit transformation to combine proportions and multilevel mixed-effect logistic regression to pool diagnostic accuracy measurements. We performed meta-regression to evaluate any significant difference between TPS and non-TPS cohorts. We included 64 studies for 99,796 combined total cytology samples, across 31 TPS and 49 non-TPS cohorts. Pooled relative distribution [95% confidence interval (CI)] of negative for high-grade urothelial carcinoma (NHGUC)/negative for malignancy (NM); atypical urothelial cells (AUC); suspicious for high-grade urothelial carcinoma (SHGUC)/suspicious for malignancy (SM); low-grade urothelial neoplasm (LGUN); and HGM categories among satisfactory cytology cases were 83.8% (80.3%–86.9%), 8.0% (6.0%–10.6%), 2.2% (1.4%–3.3%), 0.01% (0.0%–0.1%), and 4.2% (3.2%–5.5%) in TPS versus 80.8% (76.8–2.7%), 11.3% (8.6%–14.7%), 1.8% (1.2%–2.7%), 0.01% (0.0%–0.1%), and 3.3% (2.5%–4.3%) in non-TPS cohorts. Adopting TPS classification resulted in a significant increase in the frequency of NHGUC and a reduction in AUC cytology diagnoses, respectively. The AUC/HGM ratio in TPS cohort was 2.0, which showed a statistically significant difference from the atypical/HGM ratio of 4.1 in non-TPS cohort (p-value: 0.01). Moreover, the summary rate (95% CI) of LGUN called AUC on cytology significantly decreased to 20.8% (14.9%–28.3%) in the TPS compared with 34.1% (26.4%–42.8%) in non-TPS cohorts. The pooled ROHGM (95% CI) was 20.4% (6.2%–50.0%) in nondiagnostic (NDX), 15.5% (9.6%–24.2%) in NHGUC, 40.2% (30.9%–50.2%) in AUC, 80.8% (72.9%–86.8%) in SHGUC, 15.1% (5.7%–34.3%) in LGUN, and 91.4% (87.3%–94.3%) in HGM categories in TPS studies. NHGUC, AUC, SHGUC, and HGM categories were associated with HGM-LR (95% CI) of 0.2 (0.1–0.3), 0.9 (0.6–1.3), 6.9 (2.4–19.9), and 16.8 (8.3–33.8). Our results suggest that TPS 1.0 has reduced the relative frequency of AUC diagnosis, AUC/HGM ratio, and the frequency of LGUNs diagnosed as AUC on cytology. Adopting this classification has improved the clinical utility of SHGUC and HGM cytology diagnoses in ruling in high-grade lesions. However, an NHGUC diagnosis does not reliably rule out the presence of a high-grade lesion.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


