Cost-effectiveness of a group psychological intervention for postnatal depression in British south Asian women: an economic evaluation from the ROSHNI-2 trial
IF 30.8
1区 医学
Q1 PSYCHIATRY
引用次数: 0
Abstract
Background
Minority ethnic groups often face ethnocultural barriers in accessing mental health treatments. The ROSHNI-2 trial compared culturally adapted cognitive behavioural therapy (Positive Health Programme [PHP]) with treatment as usual for postnatal depression in British south Asian women. We aimed to assess the cost-effectiveness of the PHP intervention.Methods
The ROSHNI-2 trial was a multicentre, two-arm, assessor-blinded, randomised controlled trial; we conducted an economic evaluation over a 12-month period to assess the cost-effectiveness of PHP plus treatment as usual versus treatment as usual alone from the perspective of the English National Health Service and personal social services. In the trial, British south Asian women aged 16 years or older with a child aged up to 12 months, and meeting DSM-5 criteria for depression, were recruited from northwest England, Yorkshire, the East Midlands, and London. The PHP intervention involved 12 group sessions delivered by two trained bilingual facilitators, held once per week for 2 months and once per fortnight thereafter, each lasting 60–90 min. Questionnaires on depression symptoms, quality of life, and resource use were completed at baseline, 4 months (end of intervention), and 12 months after random assignment. Quality-adjusted life-years (QALYs) were used for the cost-utility analysis, and recovery from depression at 4 months (the primary clinical outcome), assessed using the Hamilton Rating Scale for Depression, informed the cost-effectiveness analysis. After the onset of the COVID-19 pandemic, the intervention was adapted for online delivery for the remaining participants. A stratified analysis compared the cost-effectiveness of online versus in-person delivery. The trial involved researchers with lived experience, and all methods, including health economic measures, were developed in consultation with service users, community members, and faith leaders. This is a preplanned analysis of the ROSHNI-2 trial, registered with ISRCTN (ISRCTN10697380).Findings
From Feb 8, 2017, to March 29, 2020, 732 eligible women were enrolled: 368 participants were randomly assigned to the PHP arm and 364 to the treatment as usual arm. The base-case intention-to-treat analysis showed that PHP significantly increased costs (£712, 95% CI 311 to 1113) and QALYs (0·036, 95% CI 0·006 to 0·067), with an incremental cost-effectiveness ratio of £19 601 (7622 to 83 772). Based on the UK National Institute for Health and Care Excellence (NICE) maximum willingness-to-pay threshold of £30 000 per QALY, the likelihood of PHP being cost-effective was 77% from a health and social care perspective. Cost per remission from depression at the 4-month follow-up was £5509 (2916 to 17 860). In a stratified analysis of 34 participants attending online sessions during the pandemic, incremental QALY effects were 0·125 (0·048 to 0·203), resulting in costs of £202 (–3906 to 10 918) per additional QALY gained.Interpretation
The average cost of PHP for postpartum women was below the lower end of the NICE threshold of £20 000–30 000 per QALY, excluding benefits to the child or potential gains such as reduced lost productivity from early remission. PHP, a culturally adapted group cognitive behavioural therapy-based intervention, might be a cost-effective intervention for postnatal depression in British south Asian women. Online PHP delivery showed promising clinical and cost-effective results for this group but requires a large-scale study.Funding
UK National Institute for Health and Care Research.英国南亚妇女产后抑郁症群体心理干预的成本-效果:来自ROSHNI-2试验的经济评估
少数民族群体在获得心理健康治疗方面往往面临民族文化障碍。ROSHNI-2试验比较了英国南亚妇女产后抑郁症的文化适应性认知行为疗法(积极健康计划[PHP])和常规治疗。我们的目的是评估PHP干预的成本效益。方法ROSHNI-2试验是一项多中心、两组、评估盲、随机对照试验;我们进行了一项为期12个月的经济评估,从英国国家卫生服务和个人社会服务的角度来评估PHP加常规治疗与单独常规治疗的成本效益。在试验中,从英格兰西北部、约克郡、东米德兰兹和伦敦招募了年龄在16岁或以上的英国南亚女性,她们有一个12个月大的孩子,符合DSM-5抑郁症标准。PHP干预包括12个小组会议,由两名训练有素的双语辅导员提供,每周举行一次,为期2个月,此后每两周举行一次,每次持续60-90分钟。在基线,4个月(干预结束)和随机分配后12个月完成抑郁症状,生活质量和资源使用问卷。使用质量调整生命年(QALYs)进行成本-效用分析,并在4个月时从抑郁症中恢复(主要临床结果),使用汉密尔顿抑郁症评定量表进行评估,为成本-效果分析提供信息。在2019冠状病毒病大流行爆发后,对其余参与者进行了在线干预。一项分层分析比较了在线授课与面对面授课的成本效益。该试验涉及具有实际经验的研究人员,所有方法,包括卫生经济措施,都是在与服务使用者、社区成员和宗教领袖协商后制定的。这是在ISRCTN注册的ROSHNI-2试验的预先计划分析(ISRCTN10697380)。从2017年2月8日到2020年3月29日,732名符合条件的女性入组:368名参与者被随机分配到PHP组,364名参与者被分配到常规治疗组。基本病例意向治疗分析显示,PHP显著增加了成本(712英镑,95% CI为311至1113)和QALYs(0.036英镑,95% CI为0.006至0.067),增量成本-效果比为19601英镑(7622至83 772英镑)。根据英国国家健康和护理卓越研究所(NICE)的最高支付意愿阈值为每个QALY 30,000英镑,从健康和社会护理的角度来看,PHP具有成本效益的可能性为77%。在4个月的随访中,每次抑郁症缓解的费用为5509英镑(2916至17860英镑)。在对大流行期间参加在线会议的34名参与者的分层分析中,质量aly的增量效应为0.125(0.048至0.0203),每获得额外的质量aly,成本为202英镑(-3906至10 918)。产后妇女的PHP平均成本低于NICE门槛的下限,即每个QALY 20,000 - 30,000英镑,不包括对儿童的好处或潜在的收益,如早期缓解减少了生产力损失。PHP是一种基于文化适应的群体认知行为疗法,可能是一种经济有效的干预英国南亚妇女产后抑郁症的方法。在线PHP交付显示了有希望的临床效果和成本效益,但需要大规模的研究。资助英国国家健康和护理研究所。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
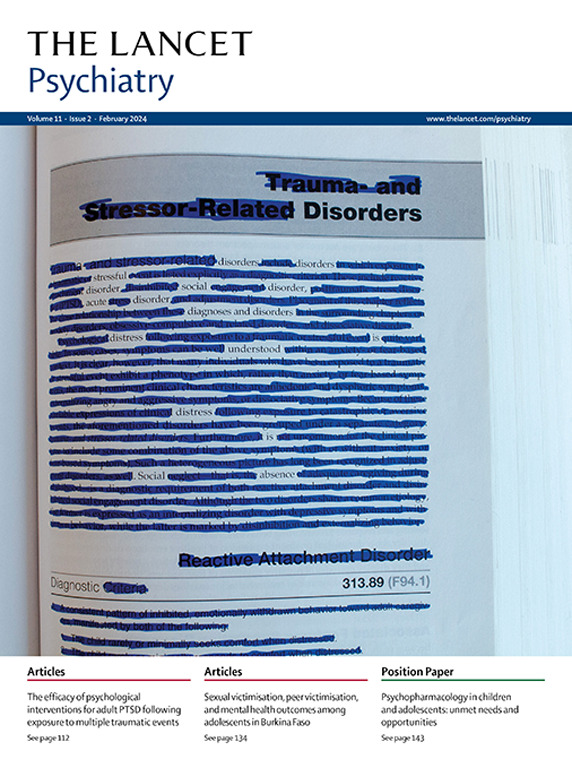
Lancet Psychiatry
PSYCHIATRY-
CiteScore
58.30
自引率
0.90%
发文量
0
期刊介绍:
The Lancet Psychiatry is a globally renowned and trusted resource for groundbreaking research in the field of psychiatry. We specialize in publishing original studies that contribute to transforming and shedding light on important aspects of psychiatric practice. Our comprehensive coverage extends to diverse topics including psychopharmacology, psychotherapy, and psychosocial approaches that address psychiatric disorders throughout the lifespan. We aim to channel innovative treatments and examine the biological research that forms the foundation of such advancements. Our journal also explores novel service delivery methods and promotes fresh perspectives on mental illness, emphasizing the significant contributions of social psychiatry.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


