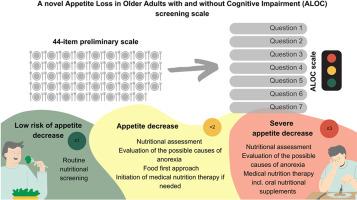
A novel appetite loss in older adults with and without cognitive impairment (ALOC) screening scale
IF 4.6
2区 医学
Q1 BEHAVIORAL SCIENCES
引用次数: 0
Abstract
Appetite is a strong determinant of nutritional status. As cognitive impairment is usually linked to alterations in eating behaviour, people with dementia might experience changes in appetite with the loss of ability to express their needs, including dietary choices and preferences. The aim of the study was to develop an appetite loss screening tool for older adults, inclusive for those with mild to moderate cognitive impairment. The study questionnaire, consisting of 44 binary items related to appetite, was employed among 127 hospitalized older patients (55.9% women, mean age 79.4 ± 7.1 years) with and without cognitive impairment (31.5% categorized as suspected mild dementia, 26.0% as suspected moderate dementia). An exploratory factor analysis was performed to identify items that constitute the final scale, with a Cronbach's alpha coefficient of 0.81. The final tool consists of seven questions, with a sensitivity of 80% and specificity of 80.6%, using the Council on Nutrition Appetite Questionnaire score as reference. Acceptability post-test was performed in 20 patients (70% women, mean age 79.6 ± 5.3 years) to test the clinical feasibility of the scale. The customized design of the scale, according to the recommendation for written materials for individuals with dementia, empowers older adults, supports diagnosis and encourages their proactivity in the treatment process. The scale was found to perform similarly in older persons with and without cognitive impairment, which renders it a versatile assessment tool.
新型认知障碍和非认知障碍老年人食欲减退(ALOC)筛查量表。
食欲是营养状况的重要决定因素。由于认知障碍通常与进食行为的改变有关,痴呆症患者可能会因为丧失表达自己需求(包括饮食选择和偏好)的能力而出现食欲变化。这项研究的目的是为老年人(包括轻度至中度认知障碍患者)开发一种食欲不振筛查工具。研究问卷由 44 个与食欲相关的二元项目组成,使用对象为 127 名住院的老年患者(55.9% 为女性,平均年龄为 79.4±7.1 岁),包括有认知障碍和无认知障碍的患者(31.5% 被归类为疑似轻度痴呆,26.0% 被归类为疑似中度痴呆)。通过探索性因子分析确定了构成最终量表的项目,Cronbach's alpha 系数为 0.81。最终工具由七个问题组成,以营养委员会食欲问卷评分为参考,灵敏度为 80%,特异性为 80.6%。对 20 名患者(70% 为女性,平均年龄为 79.6±5.3 岁)进行了可接受性后测,以检验量表的临床可行性。根据针对痴呆症患者的书面材料建议,量表采用了定制化设计,增强了老年人的能力,支持诊断并鼓励他们在治疗过程中积极主动。研究发现,该量表在有认知障碍和无认知障碍的老年人中表现相似,因此是一种通用的评估工具。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
Appetite
医学-行为科学
CiteScore
9.10
自引率
11.10%
发文量
566
审稿时长
13.4 weeks
期刊介绍:
Appetite is an international research journal specializing in cultural, social, psychological, sensory and physiological influences on the selection and intake of foods and drinks. It covers normal and disordered eating and drinking and welcomes studies of both human and non-human animal behaviour toward food. Appetite publishes research reports, reviews and commentaries. Thematic special issues appear regularly. From time to time the journal carries abstracts from professional meetings. Submissions to Appetite are expected to be based primarily on observations directly related to the selection and intake of foods and drinks; papers that are primarily focused on topics such as nutrition or obesity will not be considered unless they specifically make a novel scientific contribution to the understanding of appetite in line with the journal's aims and scope.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


