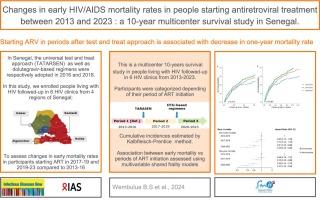
Changes in early HIV/AIDS mortality rates in people initiating antiretroviral treatment between 2013 and 2023: A 10-year multicenter survival study in Senegal
IF 2.9
4区 医学
Q2 INFECTIOUS DISEASES
引用次数: 0
Abstract
Background
HIV/AIDS-related early mortality has long been a significant challenge. Subsequent to recent policy changes and treatment advancements, we aimed to assess changes in early mortality rates in 2017–19 and 2020-23 compared to 2013–16.
Methods
This is a 10-year multicenter survival study in people living with human immunodeficiency virus having initiated ART between 2013 and 2023. We used frailty-based competing risk models to estimate adjusted early (6-month and one-year) mortality hazard ratios (HRs) in people living with HIV (PwHIV) having initiated ART in 2013–16 (comparator), 2017–19, and 2020–23.
Results
We enrolled 4006 persons of whom 2281 (56.9 %) were female; median age was 40 years (IQR: 31–50); 635 (15.9 %) were at WHO clinical stage IV and 934 (23.3 %) had a CD4 count <200 cells/mm3. Median follow-up was 80.4 months (IQR: 48.6–106.7). All in all, 463 participants died (4.37 deaths per 100 person-years), including 296 at one year of follow-up (7.4 % [95 % CI: 6.6–8.2]). ART initiation in 2016–19 and 2020–23 was associated with 27 % (adjusted HR [aHR]: 0.73; 95 % CI: 0.55–0.98) and 63 % (aHR: 0.37; 95 % CI: 0.25–0.56) reductions in one-year mortality rates, respectively, compared to the 2013–16 period.
Conclusion
Early mortality risk has significantly decreased over time in Senegal. However, the proportion of PwHIV with AIDS-defining conditions remains concerning. Continued efforts to ensure early diagnosis and prompt linkage to care are needed for more impact.
2013年至2023年期间开始接受抗逆转录病毒治疗的人群中艾滋病毒/艾滋病早期死亡率的变化:塞内加尔为期 10 年的多中心生存研究。
背景:长期以来,与艾滋病毒/艾滋病相关的早期死亡率一直是一项重大挑战。在最近的政策变化和治疗进展之后,我们旨在评估 2013-16 年和 2017-19 年与 2020-23 年相比早期死亡率的变化:这是一项为期 10 年的多中心生存研究,研究对象是 2013 年至 2023 年期间开始接受抗逆转录病毒疗法的人类免疫缺陷病毒感染者。我们使用基于虚弱的竞争风险模型来估算在 2013-16 年(比较者)、2017-19 年和 2020-23 年开始接受抗逆转录病毒疗法的艾滋病病毒感染者(PW HIV)的调整后早期(6 个月和 1 年)死亡率危险比(HRs):我们共招募了 4006 人,其中 2281 人(56.9%)为女性;年龄中位数为 40 岁(IQR:31-50);635 人(15.9%)处于 WHO 临床Ⅳ期,934 人(23.3%)的 CD4 细胞计数为 0:在塞内加尔,随着时间的推移,早期死亡风险已大大降低。然而,PW HIV 感染者中出现艾滋病定义病症的比例仍然令人担忧。需要继续努力,确保早期诊断和及时就医,以产生更大的影响。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
Infectious diseases now
Medicine-Infectious Diseases
CiteScore
7.10
自引率
2.90%
发文量
116
审稿时长
40 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


