剖腹产重症监护病房的术后护理:来自三级妇产医院的经验
IF 1.2
Q3 OBSTETRICS & GYNECOLOGY
Journal of the Turkish German Gynecological Association
Pub Date : 2023-03-15
DOI:10.4274/jtgga.galenos.2022.2021-9-27
引用次数: 0
摘要
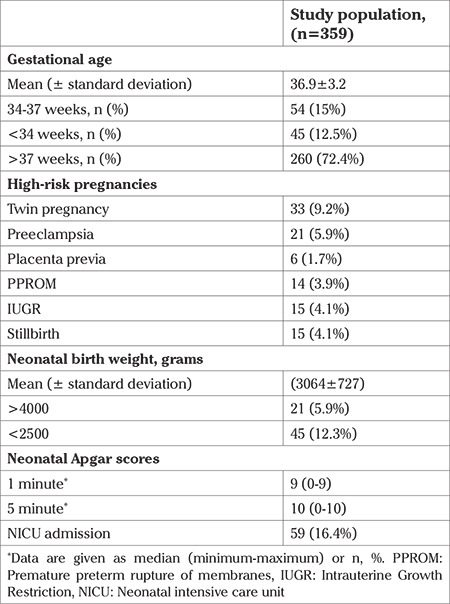
目的:探讨重症监护病房(ICU)术后前8小时随访是否有利于产后出血的早期干预。材料与方法:我院所有剖宫产术后8小时入住ICU。本研究回顾性回顾了2016年至2020年间接受药物和/或手术治疗的剖宫产后产后出血患者。结果:所有接受剖宫产的病例(n= 36396)均被回顾。359例产后出血患者被确定并纳入研究。研究组剖宫产至诊断产后出血时间为10.1±19.1小时,剖宫产至再次开腹时间为9.26±23.1小时。本院共发生剖宫产术后产妇死亡3例。在过去五年中,剖腹产患者的死亡率为每10万人3.9人。计算出我院剖宫产术后出血的发生率为1.0%,计算出产科未遂事件发生率为每1000例活产0.6例。结论:剖宫产术后前8小时在ICU随访患者,可减少因产后出血而再次剖腹手术的次数,缩短剖宫产与再次剖腹手术的间隔,降低产妇死亡率。本文章由计算机程序翻译,如有差异,请以英文原文为准。


Postoperative care in the caesarean intensive care unit: experience from a tertiary maternity hospital
Objective: The aim was to determine whether follow-up in the intensive care unit (ICU) for the postoperative first eight hours was beneficial for early intervention in postpartum hemorrhage. Material and Methods: In our hospital, all patients are admitted to the ICU for the first eight hours after cesarean section. Patients with postpartum hemorrhage after cesarean delivery who received medical and/or surgical treatment between 2016 and 2020 were reviewed in the presented study retrospectively. Results: All cases (n=36,396) who underwent cesarean delivery were reviewed. Three hundred and fifty-nine patients with postpartum hemorrhage were identified and included. In the study group the time between cesarean section and diagnosis of postpartum hemorrhage was 10.1±19.1 hours, and the time between cesarean section and re-laparotomy was 9.26±23.1 hours. A total of three maternal deaths occurred after cesarean section in our hospital. In the last five years, the mortality rate in patients delivering by cesarean section was 3.9 per 100,000. The incidence of postpartum hemorrhage in cesarean deliveries at our hospital was calculated to be 1.0%, and the rate of obstetric near-miss events was calculated to be 0.6 per 1000 live births. Conclusion: Follow-up of patients in the ICU in the first eight postoperative hours after cesarean section may result in a lower number of relaparotomies due to postpartum hemorrhage, a shortened interval between cesarean section and re-laparotomy, and a lower maternal mortality rate.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Journal of the Turkish German Gynecological Association
OBSTETRICS & GYNECOLOGY-
CiteScore
2.40
自引率
7.10%
发文量
56
期刊介绍:
Journal of the Turkish-German Gynecological Association is the official, open access publication of the Turkish-German Gynecological Education and Research Foundation and Turkish-German Gynecological Association and is published quarterly on March, June, September and December. It is an independent peer-reviewed international journal printed in English language. Manuscripts are reviewed in accordance with “double-blind peer review” process for both reviewers and authors. The target audience of Journal of the Turkish-German Gynecological Association includes gynecologists and primary care physicians interested in gynecology practice. It publishes original works on all aspects of obstertrics and gynecology. The aim of Journal of the Turkish-German Gynecological Association is to publish high quality original research articles. In addition to research articles, reviews, editorials, letters to the editor, diagnostic puzzle are also published. Suggestions for new books are also welcomed. Journal of the Turkish-German Gynecological Association does not charge any fee for article submission or processing.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


