慢性丙型肝炎患者联合肝僵硬度和Α-fetoprotein进一步超越持续病毒学反应访问作为长期肝脏相关事件的预测因子
IF 2.7
4区 医学
Q2 Medicine
Canadian Journal of Gastroenterology and Hepatology
Pub Date : 2022-07-04
eCollection Date: 2022-01-01
DOI:10.1155/2022/5201443
引用次数: 1
摘要
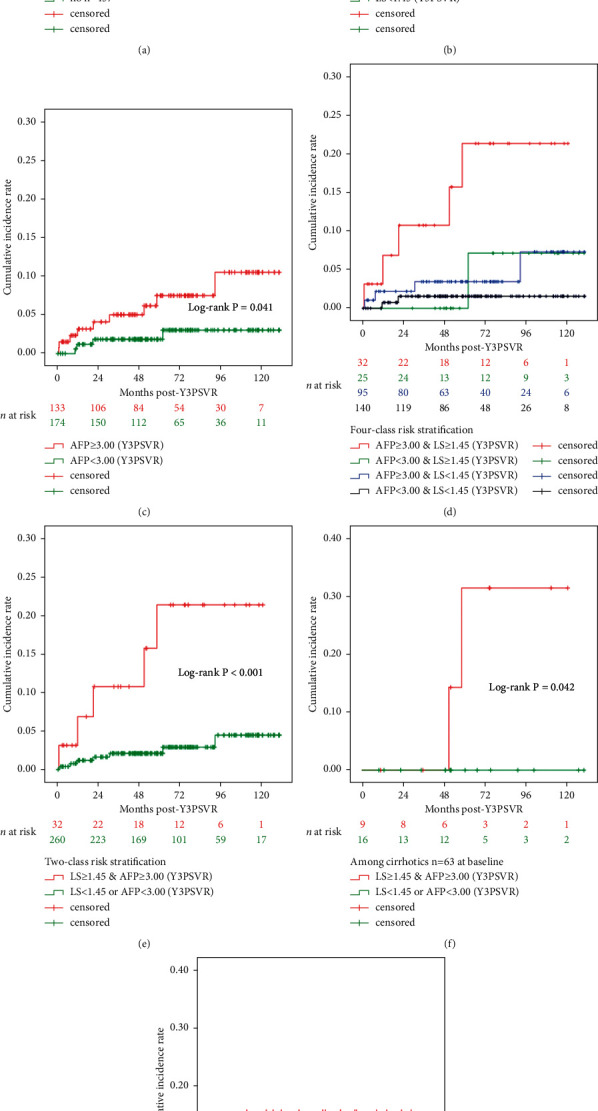
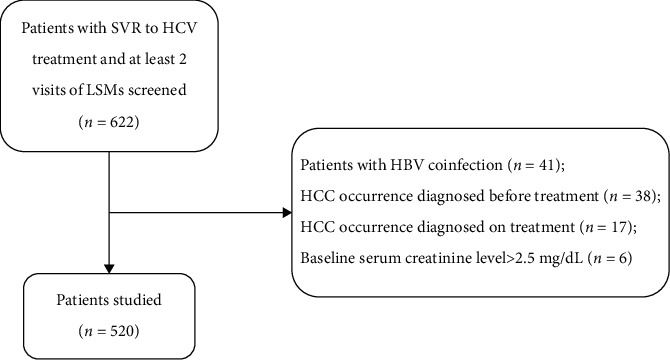
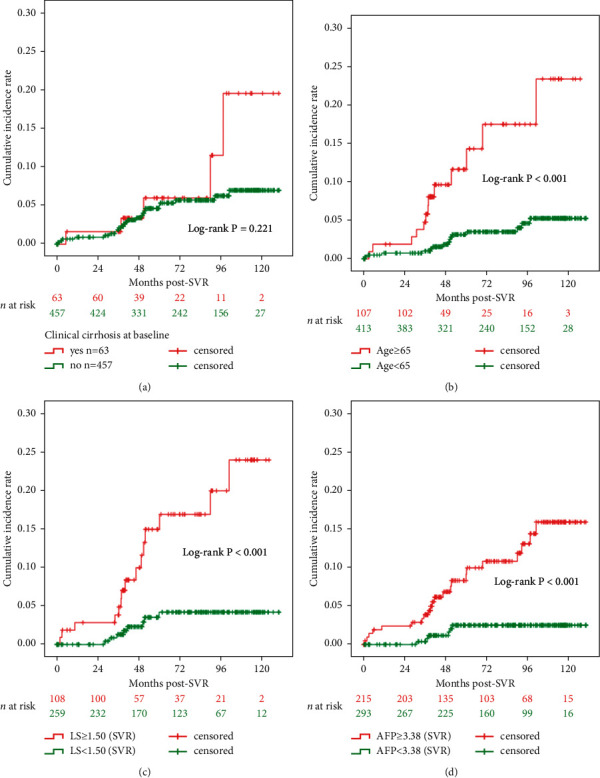
目的:慢性丙型肝炎(CHC)的长期风险分层尚未得到彻底的研究,该研究使用联合肝硬度(LS)和在基线时获得的临床相关血液检查,进一步超出了持续病毒学反应(SVR)访问。本研究回顾性调查了SVR访视后肝脏相关事件(LREs)的预后。方法:在2010年至2021年的预定随访期间,Cox回归和随机森林模型确定了可以预测LREs(包括肝细胞癌)的关键因素,包括纵向LS和无创伤检测结果。Kaplan-Meier生存分析估计了组间风险分层的重要性。结果:在接受抗病毒治疗的SVR CHC患者的整个符合条件的队列(n = 520)中,28例(5.4%)患者在中位随访6.1年(四分位数间距= 3.5-8.7)期间出现SVR后LREs。多因素Cox回归分析确定了两个显著的预测指标,即在svr后3年(Y3PSVR)基线后LREs (LRE, n = 15 / 28, 53.6%,中位随访= 4.1[1.6-6.4]年):Y3PSVR时LS(校正风险比[aHR] = 3.980, 95%可信区间[CI] = 2.085-7.597, P < 0.001)和Y3PSVR时α-胎蛋白(AFP) (aHR = 1.017, 95% CI = 1.001-1.034, P=0.034)。Y3PSVR的LS≥1.45 m/s和AFP≥3.00 ng/mL的阳性似然比分别为4.24和2.62。Kaplan-Meier分析显示,在分层亚组中,Y3PSVR时并发LS≥1.45 m/s和AFP≥3.00 ng/mL的亚组Y3PSVR后LREs的风险最高(log-rank P < 0.001)。结论:我们建议在CHC LREs的未来预测模型中联合使用并发LS和AFP。同时LS和AFP值高于SVR就诊的患者可能需要涉及强化监测的召回政策。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Combined Liver Stiffness and Α-fetoprotein Further beyond the Sustained Virologic Response Visit as Predictors of Long-Term Liver-Related Events in Patients with Chronic Hepatitis C.
Aims Long-term risk stratification using combined liver stiffness (LS) and clinically relevant blood tests acquired at the baseline further beyond the sustained virologic response (SVR) visit for chronic hepatitis C (CHC) has not been thoroughly investigated. This study retrospectively investigated the prognostics of liver-related events (LREs) further beyond the SVR visit. Methods Cox regression and random forest models identified the key factors, including longitudinal LS and noninvasive test results, that could predict LREs, including hepatocellular carcinoma, during prespecified follow-ups from 2010 to 2021. Kaplan–Meier survival analysis estimated the significance of between-group risk stratification. Results Of the entire eligible cohort (n = 520) of CHC patients with SVR to antiviral therapy, 28 (5.4%) patients developed post-SVR LREs over a median follow-up period of 6.1 years (interquartile range = 3.5–8.7). The multivariate Cox regression analysis identified two significant predictors of LREs after the year 3 post-SVR (Y3PSVR) baseline (LRE, n = 15 of 28, 53.6%, median follow-up = 4.1 [1.6–6.4] years after Y3PSVR): LS at Y3PSVR (adjusted hazard ratio [aHR] = 3.980, 95% confidence interval [CI] = 2.085–7.597, P < 0.001), and α-fetoprotein (AFP) at Y3PSVR (aHR = 1.017, 95% CI = 1.001–1.034, P=0.034). LS ≥1.45 m/s and AFP ≥3.00 ng/mL for Y3PSVR yielded positive likelihood ratios of 4.24 and 2.62, respectively. Kaplan–Meier analysis revealed that among the stratified subgroups, the subgroup with concurrent LS ≥1.45 m/s and AFP ≥3.00 ng/mL at Y3PSVR exhibited the highest risk of LREs after Y3PSVR (log-rank P < 0.001). Conclusion We recommend the combined use of concurrent LS and AFP in future prediction models for LREs in CHC. Patients with concurrently high LS and AFP values further beyond the SVR visit may require a recall policy involving intense surveillance.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Canadian Journal of Gastroenterology and Hepatology
GASTROENTEROLOGY & HEPATOLOGY-
CiteScore
4.80
自引率
0.00%
发文量
0
审稿时长
37 weeks
期刊介绍:
Canadian Journal of Gastroenterology and Hepatology is a peer-reviewed, open access journal that publishes original research articles, review articles, and clinical studies in all areas of gastroenterology and liver disease - medicine and surgery.
The Canadian Journal of Gastroenterology and Hepatology is sponsored by the Canadian Association of Gastroenterology and the Canadian Association for the Study of the Liver.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


