先前抗vegf治疗后新生血管性老年性黄斑变性持续性黄斑液的Brolucizumab。
IF 2.3
Q2 OPHTHALMOLOGY
Therapeutic Advances in Ophthalmology
Pub Date : 2021-12-13
eCollection Date: 2021-01-01
DOI:10.1177/25158414211055964
引用次数: 8
摘要
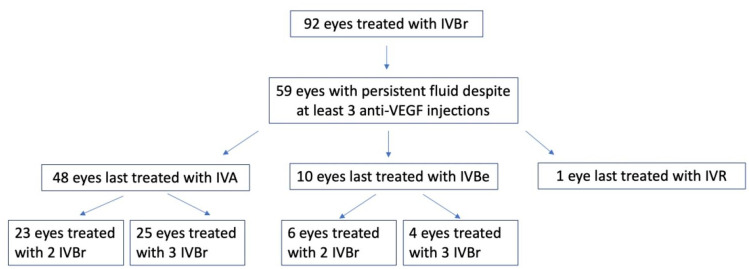
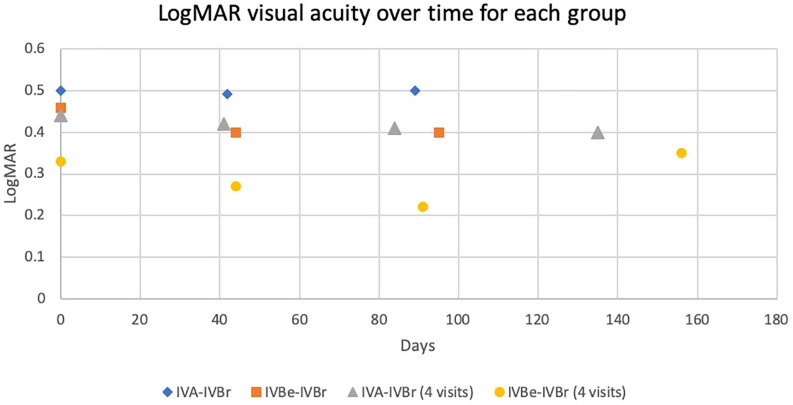
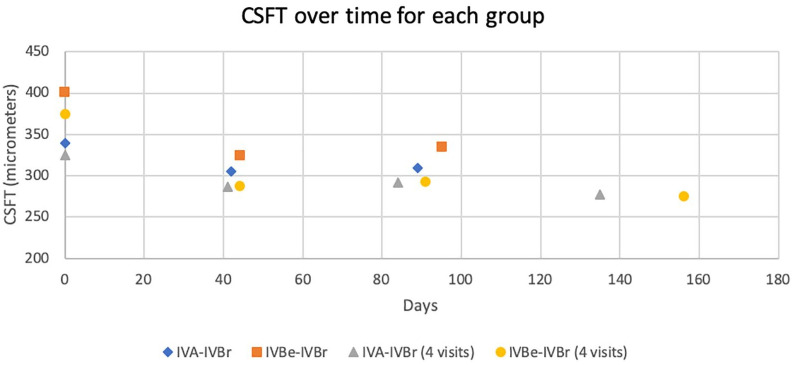
背景:一些新生血管性年龄相关性黄斑变性(nAMD)患者尽管接受了抗vegf药物治疗,但仍存在持续的视网膜内/视网膜下积液(IRF/SRF)。在这些患者中,切换到玻璃体内brolucizumab (IVBr)的疗效数据有限。目的:探讨nAMD治疗持续性IRF/SRF的解剖和视力结果。方法:回顾性系列眼部nAMD患者,最初使用阿非利赛普(IVA, n = 48)和贝伐单抗(IVBe, n = 10)治疗,然后改用IVBr治疗持续性IRF/SRF。结果:IVA-IVBr组,IVBr后平均42天,平均logMAR从0.50变化到0.49 (p = 0.73),平均CSFT从340变化到305µm (p = 0.35),平均CSFT从325变化到277µm (p = 0.001);24%的眼睛在最后一次随访时无积液,平均在最后一次IVBr后54天。IVBe-IVBr组,IVBr 1次后平均44天,平均logMAR从0.46变为0.40 (p = 0.114),平均CSFT从401变为325µm (p = 0.009);30%的眼睛没有积液,70%的眼睛持续积液但积液减少。对于完成一系列三次IVBr的四眼亚组,平均logMAR从0.33变化到0.35 (p = 0.391),平均CSFT从375改善到275µm (p = 0.001);50%的患者在最后一次随访时无积液,平均为最后一次IVBr后65天。结论:在先前接受IVA和IVBe治疗的nAMD眼睛中,切换到IVBr可显着降低持续IRF/SRF,但对视力结果没有显着影响。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Brolucizumab for persistent macular fluid in neovascular age-related macular degeneration after prior anti-VEGF treatments.
Background: Some patients with neovascular age-related macular degeneration (nAMD) have persistent intraretinal/subretinal fluid (IRF/SRF) despite being treated with anti-VEGF agents. There is limited data on efficacy of switching to intravitreal brolucizumab (IVBr) in these patients. Purpose: To determine anatomic and visual outcomes of eyes with nAMD treated with for persistent IRF/SRF. Methods: Retrospective series of eyes with nAMD treated initially with aflibercept (IVA, n = 48) and bevacizumab (IVBe, n = 10), then switched to IVBr for persistent IRF/SRF. Results: In the IVA-IVBr group, a mean of 42 days after one IVBr, mean logMAR changed from 0.50 to 0.49 (p = 0.73) and mean CSFT changed from 340 to 305 µm (p < 0.001); 31% of eyes had no fluid, 42% had persistent but reduced fluid, 25% had stable fluid, and 2% had increased fluid. For a subgroup of 25 eyes that completed a series of 3 IVBr, mean logMAR changed from 0.44 to 0.40 (p = 0.35) and mean CSFT changed from 325 to 277 µm (p = 0.001); 24% of eyes had no fluid at last follow-up, a mean of 54 days after last IVBr. In the IVBe-IVBr group, a mean of 44 days after one IVBr, mean logMAR changed from 0.46 to 0.40 (p = 0.114) and mean CSFT from 401 to 325 µm (p = 0.009); 30% of eyes had no fluid and 70% had persistent but reduced fluid. For a subgroup of four eyes that completed a series of three IVBr, mean logMAR changed from 0.33 to 0.35 (p = 0.391) and mean CSFT improved from 375 to 275 µm (p = 0.001); 50% of eyes had no fluid at last follow-up, a mean of 65 days after last IVBr. Conclusion: In nAMD eyes previously treated with IVA and IVBe, switching to IVBr significantly reduced persistent IRF/SRF but did not significantly affect visual outcomes.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Therapeutic Advances in Ophthalmology
OPHTHALMOLOGY-
CiteScore
4.50
自引率
0.00%
发文量
44
审稿时长
12 weeks
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


