猪模型模拟出血期间胸、外周和脑容积、循环和压力对PEEP的反应:一个案例研究。
摘要
呼气末正压(PEEP)是一种呼吸/通气程序,用于在肺功能受损的临床和实验病例中维持或改善呼吸。在重症监护室(ICU)应用PEEP期间,不监测体液移位运动,这对低血压患者来说尤其有趣。众所周知,脑损伤和低血压患者的脑血流量(CBF)自动调节(AR)受损,但目前还没有非侵入性的方法来评估在这些患者中实施降压复苏策略和PEEP使用的风险。生物电阻抗测量的优点是无创、连续、方便。由于它具有良好的时间分辨率,因此非常适合在重症监护室(ICU)进行监测。其未来使用的基础是建立生理相关性。在这项研究中,我们演示了在出血过程中使用生物电阻抗测量,以及在猪测量中使用PEEP。在一只麻醉的猪身上,我们对躯干和头部进行了多模式记录,包括生物电阻抗谱(EIS)、固定频率阻抗体积描记术(IPG)和双极(脑流变描记术-REG)测量,并离线处理数据。挑战(n=16)是PEEP、出血、SAP变化和CO2吸入。总测量时间为4.12小时。系统循环结果:出血导致SAP、心输出量(CO)持续下降,心率、体温、休克指数(SI)、植物Kerdo指数(KI)升高。脉冲压(PP)仅在第二次出血后下降,这与CBF-AR的损失相吻合。在PEEP激发期间,肺动脉压(PAP)随着时间和出血而增加。EIS/IPG结果:体液移位变化由EIS相关变量表征。电阻抗谱用于量化PEEP应用和模拟出血期间的血管内、间质和细胞内体积变化。血管内液体室是出血期间的主要血液来源。PEEP在第一次出血期间产生大量液体从血管内室流出,并在第二次和第三次出血后继续失血。固定频率IPG用于量化PEEP和模拟出血过程中小腿的循环反应。PEEP减少了进入小腿的动脉血流量和从小腿流出的静脉血流量。主要结果:CBF AR被评估为SAP变化的函数。出血前和中度出血后,颅内压(ICP)、REG和颈动脉血流脉冲幅度(CFa)增加。这一变化反映了血管舒张和活动性CBF-AR。在PEEP期间的额外出血后,SAP、ICP、REG、CFa信号幅度降低,表明被动性CBF-AR.1)通过模式显示的活动性AR状态的指标如下:REG(n=9,56%)、CFa(n=7,44%)和ICP(n=6,38%);2) CBF对REG的反应性优于ICP;3) 在CBF-AR活动状态下,REG和ICP的相关系数较高(R2=0.81);4) PRx和REGx反映了活动的CBF AR状态。REG的CBF-AR监测通过预防CBF降低和继发性脑损伤为患者提供了安全性。我们使用不同类型的生物阻抗仪器来识别身体不同部位的生理反应(以前没有讨论过),以及外周反应如何最终导致心输出量下降和头部变化。这些生物阻抗方法可以改善ICU监测,提高治疗的充分性,降低死亡率和发病率。
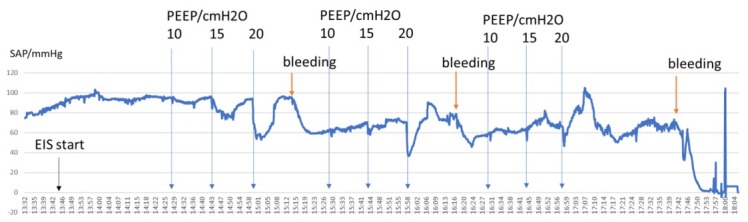
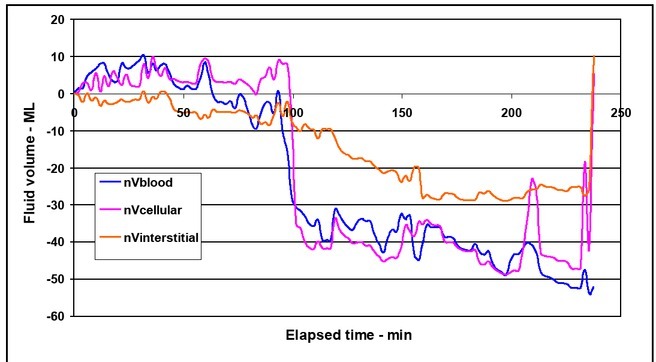
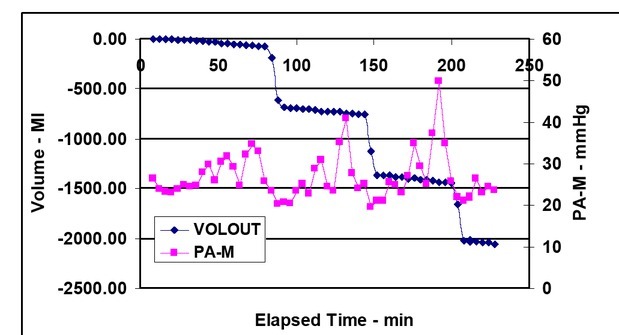
Positive end-expiratory pressure (PEEP) is a respiratory/ventilation procedure that is used to maintain or improve breathing in clinical and experimental cases that exhibit impaired lung function. Body fluid shift movement is not monitored during PEEP application in intensive care units (ICU), which would be interesting specifically in hypotensive patients. Brain injured and hypotensive patients are known to have compromised cerebral blood flow (CBF) autoregulation (AR) but currently, there is no non-invasive way to assess the risk of implementing a hypotensive resuscitation strategy and PEEP use in these patients. The advantage of electrical bioimpedance measurement is that it is noninvasive, continuous, and convenient. Since it has good time resolution, it is ideal for monitoring in intensive care units (ICU). The basis of its future use is to establish physiological correlates. In this study, we demonstrate the use of electrical bioimpedance measurement during bleeding and the use of PEEP in pig measurement. In an anesthetized pig, we performed multimodal recording on the torso and head involving electrical bioimpedance spectroscopy (EIS), fixed frequency impedance plethysmography (IPG), and bipolar (rheoencephalography - REG) measurements and processed data offline. Challenges (n=16) were PEEP, bleeding, change of SAP, and CO2 inhalation. The total measurement time was 4.12 hours. Systemic circulatory results: Bleeding caused a continuous decrease of SAP, cardiac output (CO), and increase of heart rate, temperature, shock index (SI), vegetative - Kerdo index (KI). Pulse pressure (PP) decreased only after second bleeding which coincided with loss of CBF AR. Pulmonary arterial pressure (PAP) increased during PEEP challenges as a function of time and bleeding. EIS/IPG results: Body fluid shift change was characterized by EIS-related variables. Electrical Impedance Spectroscopy was used to quantify the intravascular, interstitial, and intracellular volume changes during the application of PEEP and simulated hemorrhage. The intravascular fluid compartment was the primary source of blood during hemorrhage. PEEP produced a large fluid shift out of the intravascular compartment during the first bleeding period and continued to lose more blood following the second and third bleeding. Fixed frequency IPG was used to quantify the circulatory responses of the calf during PEEP and simulated hemorrhage. PEEP reduced the arterial blood flow into the calf and venous outflow from the calf. Head results: CBF AR was evaluated as a function of SAP change. Before bleeding, and after moderate bleeding, intracranial pressure (ICP), REG, and carotid flow pulse amplitudes (CFa) increased. This change reflected vasodilatation and active CBF AR. After additional hemorrhaging during PEEP, SAP, ICP, REG, CFa signal amplitudes decreased, indicating passive CBF AR. 1) The indicators of active AR status by modalities was the following: REG (n=9, 56 %), CFa (n=7, 44 %), and ICP (n=6, 38 %); 2) CBF reactivity was better for REG than ICP; 3) REG and ICP correlation coefficient were high (R2 = 0.81) during CBF AR active status; 4) PRx and REGx reflected active CBF AR status. CBF AR monitoring with REG offers safety for patients by preventing decreased CBF and secondary brain injury. We used different types of bioimpedance instrumentation to identify physiologic responses in the different parts of the body (that have not been discussed before) and how the peripheral responses ultimately lead to decreased cardiac output and changes in the head. These bioimpedance methods can improve ICU monitoring, increase the adequacy of therapy, and decrease mortality and morbidity.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


