非酒精性胰腺脂肪变性总是与非酒精性脂肪肝相关吗?
IF 2.5
Q2 GASTROENTEROLOGY & HEPATOLOGY
Clinical and Experimental Gastroenterology
Pub Date : 2021-06-11
eCollection Date: 2021-01-01
DOI:10.2147/CEG.S317340
引用次数: 2
摘要
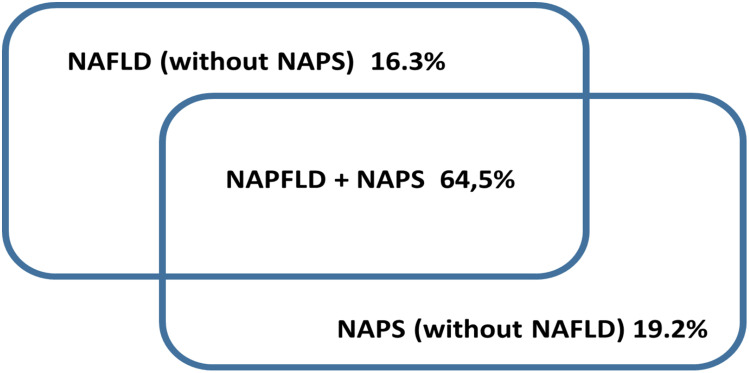
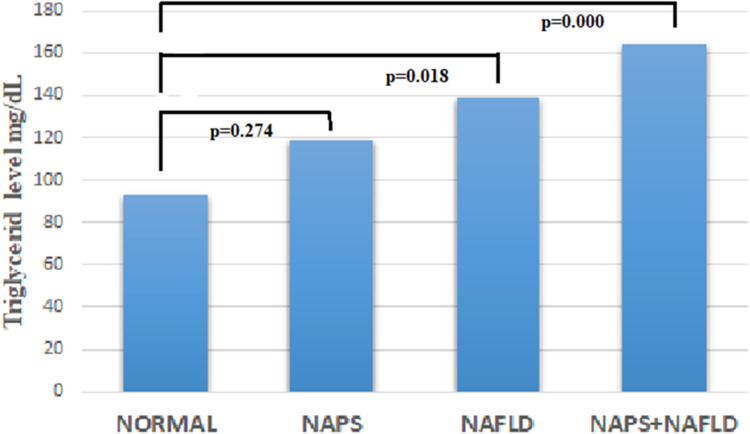
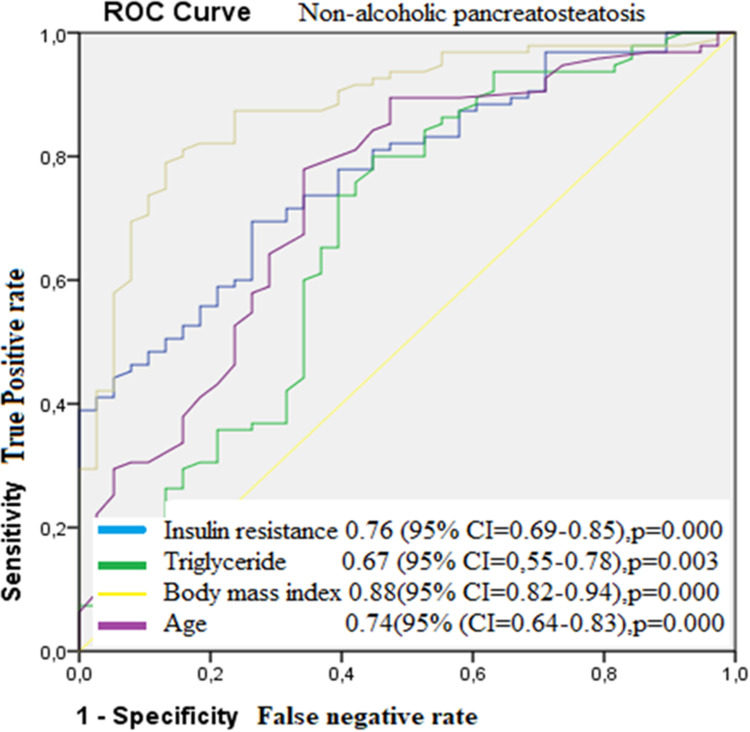
目的:在门诊组中确定非酒精性胰腺脂肪变性(NAPS)与非酒精性脂肪性肝病(NAFLD)的相关性。近年来,基于其代谢和成像特性,nap得到越来越多的认可;然而,其与NAFLD的相互作用尚不清楚。患者和方法:在这项横断面观察性研究中,纳入了345名连续无任何慢性疾病的患者,这些患者被转介给高级放射科医生进行腹部超声检查(US)。美国报告显示肝脏和胰腺回声。从医疗记录中收集患者的人口统计学、人体测量学和实验室数据。结果:总体而言,nap和NAFLD分别出现227例(65.8%)和219例(63.5%)。74例(21.4%)患者回声正常。44例(12.8%)患者为无NAFLD的脂肪变性肝,52例(15.1%)患者为无NAFLD的脂肪变性胰腺,175例(50.7%)患者为双器官脂肪变性。nap与NAFLD在脂肪变性分级上的差异为55.1%。无脂肪变性、只有NAFLD、只有nap和双器官脂肪变性的患者分别有8.7、26.7%、19%和61.3%存在胰岛素抵抗。明显的NAFLD和2级和3级脂肪变性的nap分别出现在15.3%和29.0%的研究组中。胰腺回声正常的患者中有6.8%、13.6%和28.8%存在胆囊结石,只有NAFLD和只有nap (p=0.01)。结论:基于所纳入患者的超声、临床、人口学和人体测量学特征,我们发现nap并不完全伴有非酒精性脂肪肝。尽管严重的胰腺脂肪变性,超过四分之一的病例肝脏回声正常。NAFLD患者胰岛素抵抗频率显著高于nap患者(p=0.694)。nap患者胆囊结石发生率的显著增高需要进一步的大规模研究。>50%的nap与NAFLD脂肪变性程度不一致可能反映了这两种临床实体在病理生理上的差异。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Does Nonalcoholic Pancreatic Steatosis Always Correlate with Nonalcoholic Fatty Liver Disease?
Purpose To identify the correlation of nonalcoholic pancreatic steatosis (NAPS) with nonalcoholic fatty liver disease (NAFLD) in an outpatient group. Based on its metabolic and imaging properties, NAPS has been increasingly recognized in recent years; however, its interaction with NAFLD is still not clear. Patients and Methods In this cross-sectional observational study, 345 consecutive patients without any chronic illness who were referred to the senior radiologist for abdominal ultrasound (US) were included. The US report showed hepatic and pancreatic echogenicity. The patients’ demographic, anthropometric, and laboratory data were collected from medical records. Results Overall, NAPS and NAFLD were seen in 227 (65.8%) and 219 (63.5%) patients, respectively. Normal echogenicity was noted in 74 (21.4%) patients. Forty-four patients (12.8%) had steatotic liver without NAPS, 52 (15.1%) had steatotic pancreas without NAFLD, and 175 (50.7%) had steatosis in both organs. The discordance in steatosis grading between NAPS and NAFLD was 55.1%. Insulin resistance was present in 8.7, 26.7, 19, and 61.3% of patients with no steatosis, only NAFLD, only NAPS, and steatosis in both organs, respectively. Evident NAFLD and NAPS having grade 2 and 3 steatosis were present in 15.3% and 29.0% of the study group, respectively. Cholecystolithiasis was present in 6.8, 13.6, and 28.8% of patients with normal echogenic pancreas, only NAFLD, and only NAPS, respectively (p=0.01). Conclusion Based on the ultrasonographic, clinical, demographic, and anthropometric features of the included patients, we found that NAPS did not fully accompany nonalcoholic fatty liver. Despite severe pancreatic steatosis, more than a quarter of cases had normal liver echogenicity. Insulin resistance frequency was insignificantly higher in NAFLD than NAPS (p=0.694). The significantly higher frequency of cholecystolithiasis in NAPS needs further large-scale studies. The inconsistency of steatosis degree in NAPS and NAFLD in >50% cases may reflect differences in the pathophysiology of these two clinical entities.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Clinical and Experimental Gastroenterology
GASTROENTEROLOGY & HEPATOLOGY-
CiteScore
5.10
自引率
0.00%
发文量
26
审稿时长
16 weeks
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


