创伤性脑损伤和创伤后应激障碍:战争的共病后果。
IF 2.9
Q2 NEUROSCIENCES
Neuroscience Insights
Pub Date : 2019-12-31
eCollection Date: 2019-01-01
DOI:10.1177/1179069519892933
引用次数: 18
摘要
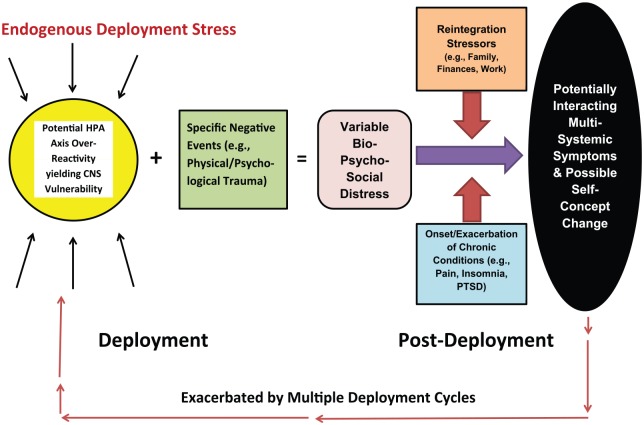
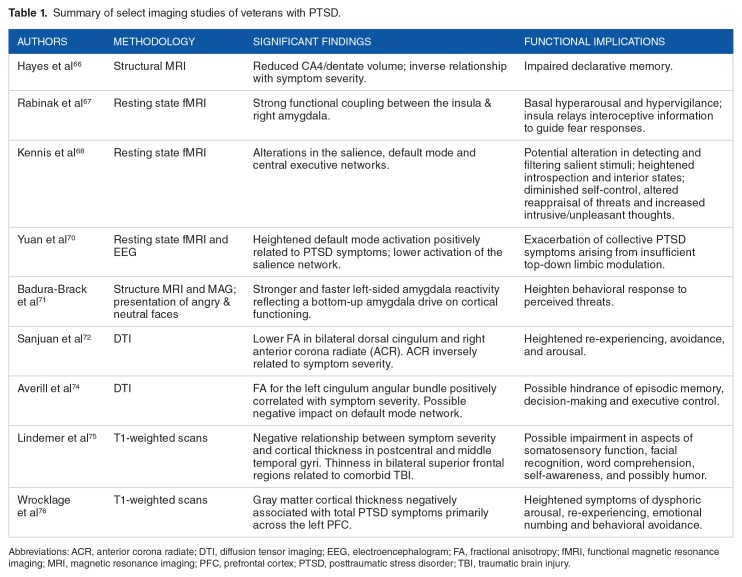
科学文献回顾支持“战争后果综合症(CWS)”在持久自由行动/伊拉克自由行动/新黎明行动的士兵。CWS的成分包括慢性疼痛和失眠、其他身体不适、创伤后应激障碍(PTSD)、焦虑、抑郁和神经心理缺陷。慢性疲劳综合征的基础是由下丘脑-垂体-肾上腺(HPA)轴失调介导和维持的慢性应激源固有的部署和级联生物事件。个体在战争中的特殊经历、重新融入部署后生活的困难,以及慢性和共病的身体、情绪和认知障碍的发作或加重,都会改变这种失调。前额叶皮层(PFC)、杏仁核和海马体之间的回路网络对战争的后果特别敏感。本综述的具体结论如下:下丘脑轴失调与士兵慢性失眠和高觉醒有关。创伤后应激障碍和爆炸相关头部损伤之间有相当多的症状重叠,很难确定这两种疾病对异常影像学研究的相对贡献。在某些情况下,创伤性脑损伤(TBI)可能直接诱发PTSD症状。虽然不是直观的,但创伤性脑损伤和脑震荡后综合征之间的关系似乎是间接的,并通过创伤后应激障碍介导。爆炸相关的或传统的头部损伤可能对神经心理功能的长期影响很小;相反,创伤后应激障碍特别能解释当前的认知缺陷。CWS的心理体验包括一场“内心战争”,士兵们继续与内心的敌人作战。CWS的成功治疗需要跨学科的护理,以解决每一个构成障碍。本文章由计算机程序翻译,如有差异,请以英文原文为准。

Traumatic Brain Injury and Posttraumatic Stress Disorder: Comorbid Consequences of War.
Scientific literature is reviewed supporting a “consequence of war syndrome (CWS)” in Operation Enduring Freedom/Operation Iraqi Freedom/Operation New Dawn soldiers. CWS constituents include chronic pain and insomnia, other physical complaints, posttraumatic stress disorder (PTSD), anxiety, depression, and neuropsychological deficits. The foundation of CWS lies with the chronic stressors inherent to deployment and the cascade of biological events mediated and maintained by hypothalamic-pituitary-adrenal (HPA) axis dysregulation. Such dysregulation is modified by the individual’s specific experiences at war, difficulty reintegrating to post-deployment life, and the onset or exacerbation of the chronic and comorbid physical, emotional, and cognitive disorders. The circuit network between the prefrontal cortex (PFC), amygdala, and hippocampus is particularly sensitive to the consequences of war. The review’s specific conclusions are as follows: HPA axis dysregulation contributes to the chronic insomnia and hyperarousal seen in soldiers. There is considerable symptom overlap between PTSD and blast-related head injury, and it is difficult to determine the relative contributions of the two disorders to abnormal imaging studies. In some cases, traumatic brain injury (TBI) may directly precipitate PTSD symptoms. While not intuitive, the relationship between TBI and postconcussion syndrome appears indirect and mediated through PTSD. Blast-related or conventional head injury may have little long-term impact on neuropsychological functioning; contrarily, PTSD particularly accounts for current cognitive deficits. The psychological experience of CWS includes a “war-within” where soldiers continue to battle an internalized enemy. Successful treatment of CWS entails transdisciplinary care that addresses each of the constituent disorders.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Neuroscience Insights
Neuroscience-Neuroscience (all)
CiteScore
6.10
自引率
0.00%
发文量
24
审稿时长
9 weeks
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


