40岁以上男性多病与未确诊的阻塞性睡眠呼吸暂停严重程度之间的关系及其对生活质量的影响
IF 1.1
Q4 PUBLIC, ENVIRONMENTAL & OCCUPATIONAL HEALTH
Global Health Epidemiology and Genomics
Pub Date : 2018-06-04
eCollection Date: 2018-01-01
DOI:10.1017/gheg.2018.9
引用次数: 22
摘要
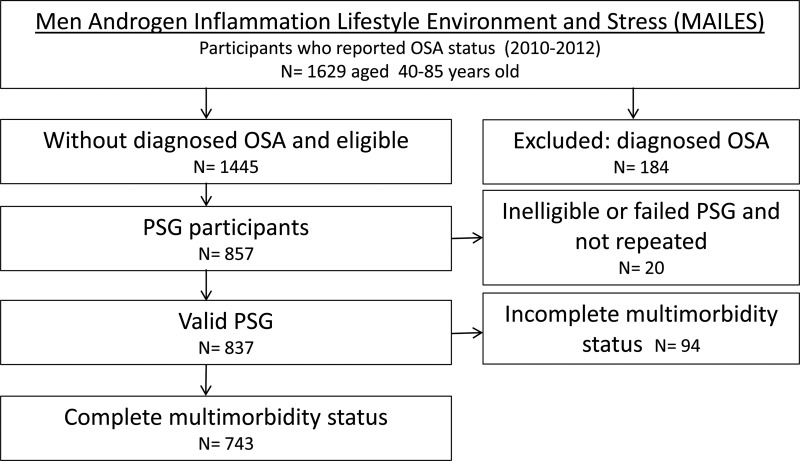
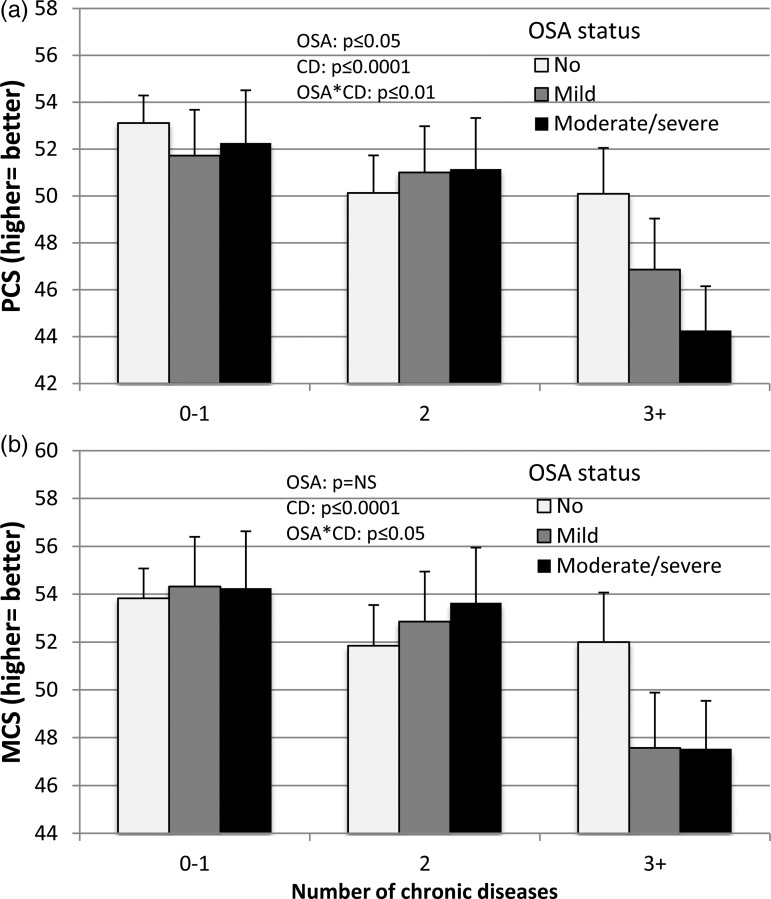
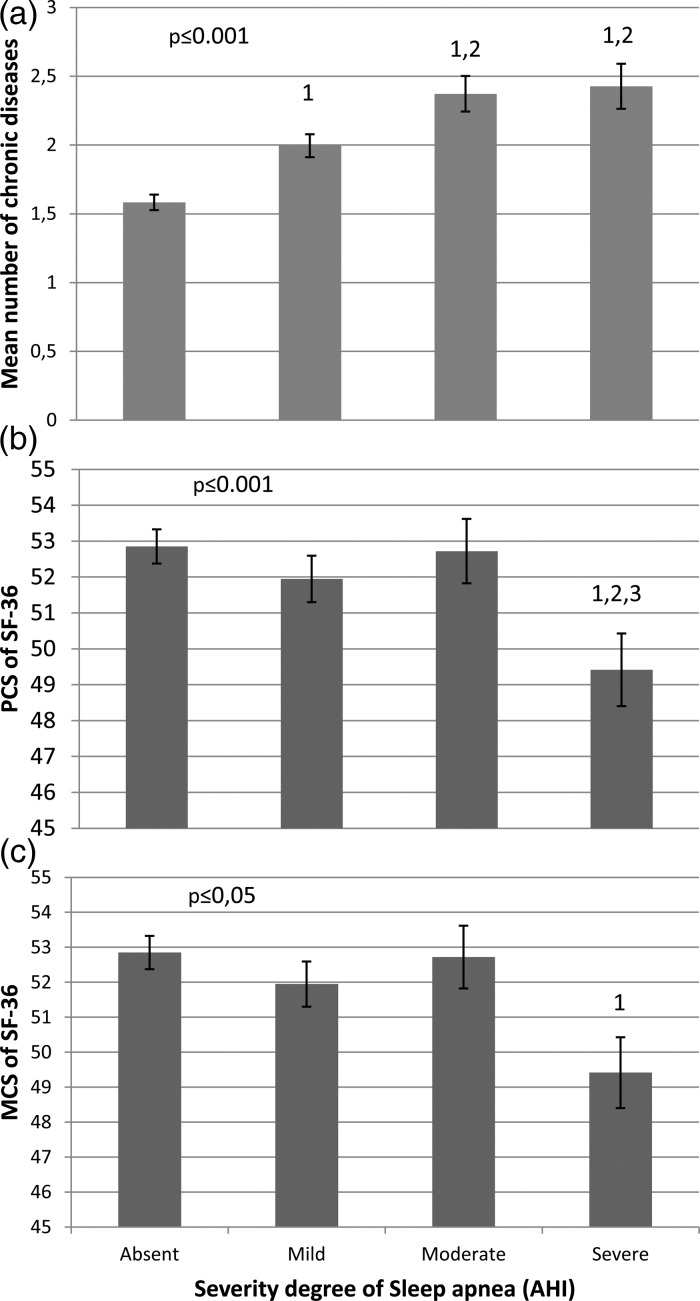
背景:多病是常见的,但对其与阻塞性睡眠呼吸暂停(OSA)的关系知之甚少。方法:参与雄激素炎症、生活方式、环境和压力研究的男性接受多导睡眠描记仪检查。慢性疾病(CDs)通过生物医学测量(糖尿病、血脂异常、高血压、肥胖)或自我报告(抑郁、哮喘、心血管疾病、关节炎)来确定。CD计数、多病性、呼吸暂停低通气指数(AHI)与OSA严重程度和生活质量(QoL)的关系心理和身体成分得分),在调整年龄后使用多项回归分析确定。结果:在参与研究的743名男性中,58%患有多病(2+ cd), 52%患有OSA(11%严重)。大约70%的多病患者患有未确诊的OSA。多发病与AHI和未确诊的OSA相关。CD计数升高与AHI值升高和OSA严重程度增加相关。结论:我们证明了OSA的存在和多病之间的独立关联,在这个代表性的社区男性样本中。这种影响在中度至重度OSA和三次或三次以上cd的男性中最为明显,当这两种情况同时出现时,似乎会产生更大的生活质量下降。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Association between multimorbidity and undiagnosed obstructive sleep apnea severity and their impact on quality of life in men over 40 years old.
Background. Multimorbidity is common but little is known about its relationship with obstructive sleep apnea (OSA). Methods. Men Androgen Inflammation Lifestyle Environment and Stress Study participants underwent polysomnography. Chronic diseases (CDs) were determined by biomedical measurement (diabetes, dyslipidaemia, hypertension, obesity), or self-report (depression, asthma, cardiovascular disease, arthritis). Associations between CD count, multimorbidity, apnea-hyponea index (AHI) and OSA severity and quality-of-life (QoL; mental & physical component scores), were determined using multinomial regression analyses, after adjustment for age. Results. Of the 743 men participating in the study, overall 58% had multimorbidity (2+ CDs), and 52% had OSA (11% severe). About 70% of those with multimorbidity had undiagnosed OSA. Multimorbidity was associated with AHI and undiagnosed OSA. Elevated CD count was associated with higher AHI value and increased OSA severity. Conclusion. We demonstrate an independent association between the presence of OSA and multimorbidity in this representative sample of community-based men. This effect was strongest in men with moderate to severe OSA and three or more CDs, and appeared to produce a greater reduction in QoL when both conditions were present together.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Global Health Epidemiology and Genomics
PUBLIC, ENVIRONMENTAL & OCCUPATIONAL HEALTH-
CiteScore
1.40
自引率
0.00%
发文量
10
审稿时长
20 weeks
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


