Kate E. Best, Judith Rankin
下载PDF
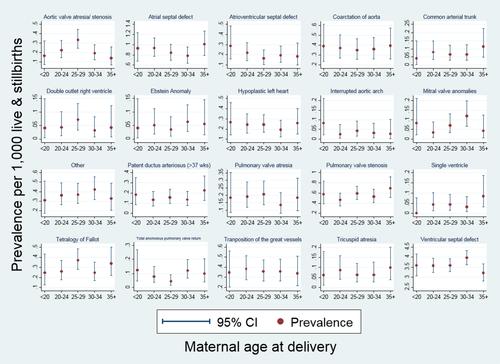
{"title":"高龄产妇是先天性心脏病的危险因素吗?","authors":"Kate E. Best, Judith Rankin","doi":"10.1002/bdra.23507","DOIUrl":null,"url":null,"abstract":"<div>\n \n <section>\n \n <h3> Background</h3>\n \n <p>Studies have reported that advanced maternal age is a risk factor for congenital heart disease (CHD), but none of these have been performed in the United Kingdom. Currently, women in the United Kingdom are not referred for specialist fetal echocardiography based on maternal age alone. The aim of this study is to examine the association between maternal age at delivery and CHD prevalence in the North of England.</p>\n </section>\n \n <section>\n \n <h3> Methods</h3>\n \n <p>Singleton cases of CHD notified to the Northern Congenital Abnormality Survey and born between January 1, 1998, to December 31, 2013, were included. Cases with chromosomal anomalies were excluded. The relative risk (RR) of CHD according to maternal age at delivery was estimated using Poisson regression.</p>\n </section>\n \n <section>\n \n <h3> Results</h3>\n \n <p>There were 4024 singleton cases of nonchromosomal CHD, giving a prevalence of 8.1 (95% confidence interval [CI], 7.8–8.3) per 1000 live and stillbirths. There was no association between maternal age at delivery and CHD prevalence (<i>p</i> = 0.97), with no evidence of an increased risk of CHD in mothers aged ≥35 compared to aged 25 to 29 (RR = 0.99; 95% CI, 0.89–1.09). There were no significant associations between maternal age at delivery and severity III CHD (<i>p</i> = 0.84), severity II CHD (<i>p</i> = 0.74), or severity I CHD (<i>p</i> = 0.66), although there was a slight increased risk of severity I CHD in mothers aged ≥35 (RR = 1.27; 95% CI, 0.83–1.95).</p>\n </section>\n \n <section>\n \n <h3> Conclusion</h3>\n \n <p>We found little evidence that advanced maternal age is a risk factor for CHD. There is no evidence that women in the United Kingdom should be referred for specialist prenatal cardiac screening based on their age. Birth Defects Research (Part A) 106:461–467, 2016. © 2016 Wiley Periodicals, Inc.</p>\n </section>\n </div>","PeriodicalId":8983,"journal":{"name":"Birth defects research. Part A, Clinical and molecular teratology","volume":"106 6","pages":"461-467"},"PeriodicalIF":0.0000,"publicationDate":"2016-06-14","publicationTypes":"Journal Article","fieldsOfStudy":null,"isOpenAccess":false,"openAccessPdf":"https://sci-hub-pdf.com/10.1002/bdra.23507","citationCount":"41","resultStr":"{\"title\":\"Is advanced maternal age a risk factor for congenital heart disease?\",\"authors\":\"Kate E. Best, Judith Rankin\",\"doi\":\"10.1002/bdra.23507\",\"DOIUrl\":null,\"url\":null,\"abstract\":\"<div>\\n \\n <section>\\n \\n <h3> Background</h3>\\n \\n <p>Studies have reported that advanced maternal age is a risk factor for congenital heart disease (CHD), but none of these have been performed in the United Kingdom. Currently, women in the United Kingdom are not referred for specialist fetal echocardiography based on maternal age alone. The aim of this study is to examine the association between maternal age at delivery and CHD prevalence in the North of England.</p>\\n </section>\\n \\n <section>\\n \\n <h3> Methods</h3>\\n \\n <p>Singleton cases of CHD notified to the Northern Congenital Abnormality Survey and born between January 1, 1998, to December 31, 2013, were included. Cases with chromosomal anomalies were excluded. The relative risk (RR) of CHD according to maternal age at delivery was estimated using Poisson regression.</p>\\n </section>\\n \\n <section>\\n \\n <h3> Results</h3>\\n \\n <p>There were 4024 singleton cases of nonchromosomal CHD, giving a prevalence of 8.1 (95% confidence interval [CI], 7.8–8.3) per 1000 live and stillbirths. There was no association between maternal age at delivery and CHD prevalence (<i>p</i> = 0.97), with no evidence of an increased risk of CHD in mothers aged ≥35 compared to aged 25 to 29 (RR = 0.99; 95% CI, 0.89–1.09). There were no significant associations between maternal age at delivery and severity III CHD (<i>p</i> = 0.84), severity II CHD (<i>p</i> = 0.74), or severity I CHD (<i>p</i> = 0.66), although there was a slight increased risk of severity I CHD in mothers aged ≥35 (RR = 1.27; 95% CI, 0.83–1.95).</p>\\n </section>\\n \\n <section>\\n \\n <h3> Conclusion</h3>\\n \\n <p>We found little evidence that advanced maternal age is a risk factor for CHD. There is no evidence that women in the United Kingdom should be referred for specialist prenatal cardiac screening based on their age. Birth Defects Research (Part A) 106:461–467, 2016. © 2016 Wiley Periodicals, Inc.</p>\\n </section>\\n </div>\",\"PeriodicalId\":8983,\"journal\":{\"name\":\"Birth defects research. Part A, Clinical and molecular teratology\",\"volume\":\"106 6\",\"pages\":\"461-467\"},\"PeriodicalIF\":0.0000,\"publicationDate\":\"2016-06-14\",\"publicationTypes\":\"Journal Article\",\"fieldsOfStudy\":null,\"isOpenAccess\":false,\"openAccessPdf\":\"https://sci-hub-pdf.com/10.1002/bdra.23507\",\"citationCount\":\"41\",\"resultStr\":null,\"platform\":\"Semanticscholar\",\"paperid\":null,\"PeriodicalName\":\"Birth defects research. Part A, Clinical and molecular teratology\",\"FirstCategoryId\":\"1085\",\"ListUrlMain\":\"https://onlinelibrary.wiley.com/doi/10.1002/bdra.23507\",\"RegionNum\":0,\"RegionCategory\":null,\"ArticlePicture\":[],\"TitleCN\":null,\"AbstractTextCN\":null,\"PMCID\":null,\"EPubDate\":\"\",\"PubModel\":\"\",\"JCR\":\"Q\",\"JCRName\":\"Medicine\",\"Score\":null,\"Total\":0}","platform":"Semanticscholar","paperid":null,"PeriodicalName":"Birth defects research. Part A, Clinical and molecular teratology","FirstCategoryId":"1085","ListUrlMain":"https://onlinelibrary.wiley.com/doi/10.1002/bdra.23507","RegionNum":0,"RegionCategory":null,"ArticlePicture":[],"TitleCN":null,"AbstractTextCN":null,"PMCID":null,"EPubDate":"","PubModel":"","JCR":"Q","JCRName":"Medicine","Score":null,"Total":0}
引用次数: 41
引用
批量引用

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


