在近一半的转诊患者中,专门的肉瘤病理检查对于确证诊断是必要的
IF 2.7
2区 医学
Q1 SURGERY
引用次数: 0
摘要
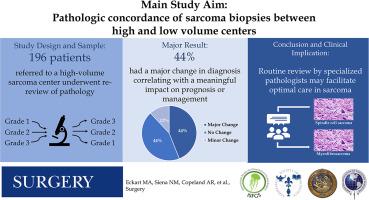
专业中心已被证明可以改善肉瘤患者的生存率和功能预后。本研究的目的是确定高、低体积肉瘤中心病理诊断变化的比率和临床影响。方法:我们对加州大学洛杉矶分校多学科肉瘤会议上讨论的患者进行了回顾性研究。来自外部机构的病理报告和随后正式的加州大学洛杉矶分校病理检查的患者被纳入。在1350例病例和877例独特患者中,196例患者被确定为分析对象。主要结果是评估高和低体积肉瘤中心病理诊断的一致性。一致性被定义为完全一致,轻微不一致,或主要不一致的原始诊断和复查之间的肉瘤病理专家。结果纳入研究的196例患者中,44%的患者病理检查完全一致,12%有轻微不一致,44%有严重不一致。主要不一致包括良/恶性不匹配(n = 23/87, 26%)、组织学亚型差异(n = 25/87, 29%)、从非诊断性到诊断性的变化(n = 34/87, 39%)和主要分级差异(n = 5/87, 6%)。在排除其他高容量中心(n = 18)后,主要不一致率增加到48% (n = 85/178)。结论:近一半(44%)的患者转诊到大容量肉瘤中心后,其诊断发生重大改变,影响预后或治疗计划。对所有潜在的肉瘤诊断进行病理复查的协调系统可以促进这些罕见恶性肿瘤患者的最佳治疗。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Dedicated review of sarcoma pathology is necessary for corroborative diagnosis in nearly one half of referred patients
Background
Specialized centers have been shown to improve survival and functional outcomes in patients with sarcoma. The objective of this study was to determine the rate and clinical impact of changes in pathologic diagnosis between high- and low-volume sarcoma centers.
Methods
We performed a retrospective review of patients discussed at UCLA Multidisciplinary Sarcoma Conference over 1 year. Patients with a pathology report from an outside facility and subsequent formal UCLA pathology review were included. Of 1,350 cases and 877 unique patients presented, 196 patients were identified for analysis. The primary outcome was to assess concordance between pathologic diagnosis at high- and low-volume sarcoma centers. Concordance was defined as either full concordance, minor discordance, or major discordance between the original diagnosis and review by a sarcoma pathology specialist.
Results
Of the 196 patients who were included in this study, 44% had full concordance on review of their pathology, 12% had minor discordance, and 44% had major discordance. Major discordance included benign/malignant mismatch (n = 23/87, 26%), discrepancy in histologic subtype (n = 25/87, 29%), change from nondiagnostic to diagnostic (n = 34/87, 39%) and major grading discrepancy (n = 5/87, 6%). After excluding other high-volume centers (n = 18), the major discordance rate increased to 48% (n = 85/178).
Conclusion
Nearly one half (44%) of patients had a major change to their diagnosis that would affect prognosis or treatment plan after referral to a high-volume sarcoma center. A coordinated system for pathologic re-review for all potential sarcoma diagnoses could facilitate optimal management of patients with these rare malignancies.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Surgery
医学-外科
CiteScore
5.40
自引率
5.30%
发文量
687
审稿时长
64 days
期刊介绍:
For 66 years, Surgery has published practical, authoritative information about procedures, clinical advances, and major trends shaping general surgery. Each issue features original scientific contributions and clinical reports. Peer-reviewed articles cover topics in oncology, trauma, gastrointestinal, vascular, and transplantation surgery. The journal also publishes papers from the meetings of its sponsoring societies, the Society of University Surgeons, the Central Surgical Association, and the American Association of Endocrine Surgeons.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


