甲状腺切除术后经皮喉超声检查:诊断准确性和学习曲线。
IF 2.7
2区 医学
Q1 SURGERY
引用次数: 0
摘要
简介:声带麻痹是甲状腺切除术后罕见的并发症,约占手术的3%至4%。柔性喉镜是评估术后声带活动的金标准,但由于费用、不适和可用性,其使用受到限制。经皮喉部超声检查已发展成为一种无创和广泛可用的替代方法。材料和方法:我们对接受头颈外科手术的全部或部分甲状腺切除术的成年患者进行了前瞻性横断面研究。手术医生术后行经皮喉部超声检查,并与盲法喉镜检查结果进行比较。计算敏感性、特异性、预测值和似然比。对于非诊断性测试,评估了最佳和最坏情况。还进行了学习曲线研究。结果:共纳入146例患者239条高危神经。有声带麻痹危险的神经占2.1%。经皮喉部超声检查显示敏感性为80%,特异性范围为94.4%至99.6%,具体取决于临床情况。阴性预测值仍然很高(99.6%),而阳性预测值在23.5%至80%之间。大约50次考试后,学习曲线趋于稳定,平均考试时间为26.9秒。结论:经皮喉部超声检查诊断准确率高,诊断效率高,是甲状腺切除术患者术后声带评价的一种经济有效的方法。本文章由计算机程序翻译,如有差异,请以英文原文为准。
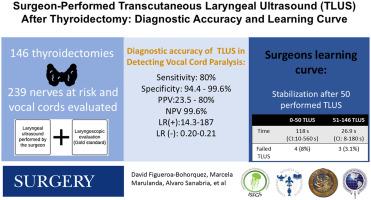
Surgeon-performed transcutaneous laryngeal ultrasonography after thyroidectomy: Diagnostic accuracy and learning curve
Introduction
Vocal cord paralysis is an uncommon complication after thyroidectomy, reported in approximately 3% to 4% of procedures. Flexible laryngoscopy is the gold standard for assessing postoperative vocal cord mobility, but its usage is limited because of expense, discomfort, and availability. Transcutaneous laryngeal ultrasonography has evolved as a noninvasive and widely available alternative.
Materials and Methods
We conducted a prospective cross-sectional study on adult patients receiving total or partial thyroidectomy by head and neck surgeons. The operating surgeon performed transcutaneous laryngeal ultrasonography postoperatively and compared the results to a blinded laryngoscopic examination. The sensitivity, specificity, predictive value, and likelihood ratios were calculated. For nondiagnostic tests, best- and worst-case scenarios were evaluated. A learning curve study was also conducted.
Results
A total of 146 patients with 239 nerves at risk were included. Vocal cord paralysis was observed in 2.1% of nerves at risk. Transcutaneous laryngeal ultrasonography demonstrated a sensitivity of 80% and a specificity ranging from 94.4% to 99.6%, depending on the clinical scenario. The negative predictive value remained high (99.6%), whereas the positive predictive value ranged from 23.5% to 80%. After about 50 examinations, the learning curve stabilized, and the median examination length was 26.9 seconds.
Conclusion
Surgeons may conduct transcutaneous laryngeal ultrasonography with good diagnostic accuracy and efficiency, making it a cost-effective technique for postoperative vocal cord evaluation in thyroidectomy patients.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Surgery
医学-外科
CiteScore
5.40
自引率
5.30%
发文量
687
审稿时长
64 days
期刊介绍:
For 66 years, Surgery has published practical, authoritative information about procedures, clinical advances, and major trends shaping general surgery. Each issue features original scientific contributions and clinical reports. Peer-reviewed articles cover topics in oncology, trauma, gastrointestinal, vascular, and transplantation surgery. The journal also publishes papers from the meetings of its sponsoring societies, the Society of University Surgeons, the Central Surgical Association, and the American Association of Endocrine Surgeons.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


