围手术期多重耐药细菌影响胰腺手术后的临床结果:错过了抗生素预防的目标。
IF 2.7
2区 医学
Q1 SURGERY
引用次数: 0
摘要
背景:耐多药细菌是围手术期医学关注的主要问题。术前定植和术后多药耐药细菌检测对胰腺手术结果的影响程度在很大程度上是未知的。微生物组分析为适当的围手术期抗生素预防提供了见解。方法:这是一项回顾性、单中心队列研究,纳入了2018年1月至2022年12月期间接受择期胰腺手术的患者,并进行了一整套术前筛查拭子。结果:212例患者围手术期耐多药阴性168例(79.25%),耐多药阳性44例(20.75%)。其中术前检出耐多药菌19例,术后检出耐多药菌25例。未观察到基线特征的差异。包括血白细胞和c反应蛋白在内的炎症参数在多药耐药阳性患者围手术期升高。与耐多药阴性患者相比,耐多药阳性患者的术后结果明显受损,包括胰瘘(B/C级)、胰腺切除术后出血和再手术的发生率更高(均P < 0.0001)。主要并发症发生率、重症监护时间和住院时间均增加(P < 0.0001)。多药耐药阳性患者胰瘘发展为出血和再手术的比例尤其高(37.84% vs 3.92%; P < 0.0001)。亚组分析显示,术前多药耐药阳性患者和术后多药耐药阳性患者的术后结局无差异。胰腺手术围手术期常用抗生素甲硝唑/第二代头孢菌素或哌拉西林/他唑巴坦的固有或获得性耐药率较高。结论:术前和术后多药耐药菌定植对术后预后均有不良影响。胰瘘是多药耐药阳性患者严重发病的重要原因。高危胰腺手术患者应考虑术前去菌落、围手术期广谱抗生素预防及术后持续抗生素治疗。本文章由计算机程序翻译,如有差异,请以英文原文为准。
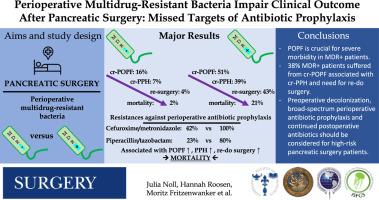
Perioperative multidrug-resistant bacteria impair clinical outcome after pancreatic surgery: Missed targets of antibiotic prophylaxis
Background
Multidrug-resistant bacteria represent major concerns in perioperative medicine. The extent to which preoperative colonization and postoperative detection of multidrug-resistant bacteria affect outcome in pancreatic surgery is largely unknown. Microbiome analyses provide insights into appropriate perioperative antibiotic prophylaxis.
Methods
This was a retrospective, single-center cohort study of patients who underwent elective pancreatic surgery between January 2018 and December 2022 with a complete set of preoperative screening swabs.
Results
Of 212 patients, n = 168 (79.25%) were classified as multidrug-resistant negative, whereas 44 (20.75%) were tested multidrug-resistant positive perioperatively. Among these, 19 had preoperative detection of multidrug-resistant bacteria and 25 had postoperative detection of multidrug-resistant bacteria. No differences in baseline characteristics were observed. Inflammatory parameters, including blood leukocytes and C-reactive protein, were elevated perioperatively in patients who were multidrug-resistant positive. Postoperative outcomes were significantly impaired in patients who were multidrug-resistant positive compared with those who were multidrug-resistant negative, including greater rates of pancreatic fistula (grade B/C), postpancreatectomy hemorrhage, and reoperation (all P < .0001). Major complication rates, length of intensive care, and in-hospital stay were increased (all P < .0001). Progression of pancreatic fistula to hemorrhage and reoperation was particularly high in patients who were multidrug-resistant positive (37.84% vs 3.92%; P < .0001). Subgroup analyses revealed no differences in postoperative outcomes between patients who were preoperatively tested multidrug-resistant positive and those who were postoperatively tested multidrug-resistant positive. High intrinsic or acquired bacterial resistance rates were observed against commonly used perioperative antibiotics in pancreatic surgery, including metronidazole/second-generation cephalosporins or piperacillin/tazobactam.
Conclusion
Both preoperative and postoperative colonization with multidrug-resistant bacteria have deleterious effects on postoperative outcomes. Pancreatic fistula is a crucial cause for severe morbidity in patients who are multidrug-resistant positive. Preoperative decolonization, broad-spectrum perioperative antibiotic prophylaxis, and continued postoperative antibiotics should be considered for high-risk pancreatic surgery patients.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Surgery
医学-外科
CiteScore
5.40
自引率
5.30%
发文量
687
审稿时长
64 days
期刊介绍:
For 66 years, Surgery has published practical, authoritative information about procedures, clinical advances, and major trends shaping general surgery. Each issue features original scientific contributions and clinical reports. Peer-reviewed articles cover topics in oncology, trauma, gastrointestinal, vascular, and transplantation surgery. The journal also publishes papers from the meetings of its sponsoring societies, the Society of University Surgeons, the Central Surgical Association, and the American Association of Endocrine Surgeons.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


