肝脂质含量轻度升高的特点是胰岛素敏感性降低
IF 7.5
1区 医学
Q1 GASTROENTEROLOGY & HEPATOLOGY
引用次数: 0
摘要
背景和目的最近,在一项大型人群试验的基础上,提出了一个新的正常肝脏脂质含量临界值≤1.85%。在该研究中,与肝脂含量≤1.85%的人群相比,肝脂含量在1.86%至目前使用的磁共振波谱特异性上限5.56%之间的人群胰岛素敏感性较低(胰岛素抵抗的稳态模型评估更高[HOMA-IR])。我们的目的是在这些发现的基础上,评估低(LL≤1.85%)或轻度升高(MEL; >;1.85%和≤5.56%)肝脏脂质的个体之间组织特异性胰岛素敏感性的差异。方法结合以往研究的数据,本横断面研究纳入了202名无糖尿病的欧洲白人。用磁共振波谱法测定肝脏脂质。采用高胰岛素-血糖钳钳联合[18F]氟脱氧葡萄糖正电子发射断层扫描测定内源性葡萄糖生成(EGP, N = 96),空腹游离脂肪酸与胰岛素的产物测定脂肪组织胰岛素抵抗(N = 197)。采用核磁共振代谢组学方法测定血清代谢物(N = 152)。结果MEL组高胰岛素血症时EGP升高(2.7[-0.4;7.5]比-0.2 [-4.3;5.3]μmol/kg/min, p = 0.041),空腹脂肪组织胰岛素抵抗升高(28.4[16.6;37.5]比17.6 [9.6;26.9]pmol/L × mmol/L, p = 0.037)。此外,与LL组相比,血清甘油三酯和支链氨基酸升高(错误发现率<;0.05)。结论与LL患者相比,MEL患者肝脏和脂肪组织胰岛素敏感性较低,代谢物发生不良变化。这些发现支持了欧洲白人正常肝脏脂质较低的上限。此外,数据表明,高胰岛素血症期间EGP抑制受损和脂解胰岛素抵抗是全身性胰岛素抵抗级联的早期特征。影响和意义长期以来,人们都知道肝脏脂质含量的显著增加与心血管危险因素的增加有关。从研究人员和临床医生的角度来看,重要的是要知道,即使是轻微升高的肝脏脂质含量也与许多不良的代谢变化有关。需要进一步的研究来证实,在脂肪肝发展的早期干预生活方式,如有必要,在早期阶段进行药物治疗,是否有助于预防未来的代谢性疾病。临床试验注册该研究已在ClinicalTrials.gov注册(NCT03310502)。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Mildly elevated liver lipid content is characterised by reduced insulin sensitivity
Background & Aims
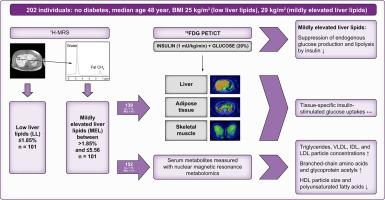
Recently, a new cut-off of ≤1.85% was proposed for normal liver lipid content based on a large population trial. In that study, people having liver lipid between 1.86% and the currently used magnetic resonance spectroscopy-specific upper limit of 5.56% had lower insulin sensitivity (higher homeostatic model assessment for insulin resistance [HOMA-IR]) when compared with people with ≤1.85% of liver lipid. We aimed to build upon these findings by evaluating differences in tissue-specific insulin sensitivity between individuals having low (LL; ≤1.85%) or mildly elevated (MEL; >1.85% and ≤5.56%) liver lipids.
Methods
Combining data from previous studies, 202 White European individuals without diabetes were included in this cross-sectional study. Liver lipids were measured with magnetic resonance spectroscopy. Endogenous glucose production (EGP; N = 96) was measured by hyperinsulinaemic–euglycaemic clamp combined with [18F]fluorodeoxyglucose positron emission tomography, and adipose tissue insulin resistance by the product of fasting free fatty acids and insulin (N = 197). Serum metabolites were measured using nuclear magnetic resonance metabolomics (N = 152).
Results
The MEL group had higher EGP during hyperinsulinemia (2.7 [-0.4; 7.5] vs. -0.2 [-4.3; 5.3] μmol/kg/min, p = 0.041) and higher adipose tissue insulin resistance at fasting (28.4 [16.6; 37.5] vs. 17.6 [9.6; 26.9] pmol/L × mmol/L, p = 0.037) compared with the LL group. In addition, serum triglycerides and branched-chain amino acids were elevated (false discovery rate <0.05) compared with the LL group.
Conclusions
People with MEL had lower hepatic and adipose tissue insulin sensitivity and adverse changes in metabolites when compared with people with LL. These findings support a lower upper limit for normal liver lipids in White Europeans. In addition, the data indicate that impaired suppression of EGP during hyperinsulinaemia and insulin resistance of lipolysis are early features in the cascade of systemic insulin resistance.
Impact and implications
It has long been known that a substantially increased liver lipid content is connected to an increase in cardiovascular risk factors. From the perspective of both researchers and clinicians, it is important to know that even slightly elevated liver lipid content is associated with many adverse metabolic changes. Further research is needed to confirm if intervening early in the development of fatty liver with lifestyle intervention and, if necessary, drug treatment at an early stage, provide benefit for the prevention of metabolic diseases in the future.
Clinical Trials Registration
The study has been registered at ClinicalTrials.gov (NCT03310502).
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

JHEP Reports
GASTROENTEROLOGY & HEPATOLOGY-
CiteScore
12.40
自引率
2.40%
发文量
161
审稿时长
36 days
期刊介绍:
JHEP Reports is an open access journal that is affiliated with the European Association for the Study of the Liver (EASL). It serves as a companion journal to the highly respected Journal of Hepatology.
The primary objective of JHEP Reports is to publish original papers and reviews that contribute to the advancement of knowledge in the field of liver diseases. The journal covers a wide range of topics, including basic, translational, and clinical research. It also focuses on global issues in hepatology, with particular emphasis on areas such as clinical trials, novel diagnostics, precision medicine and therapeutics, cancer research, cellular and molecular studies, artificial intelligence, microbiome research, epidemiology, and cutting-edge technologies.
In summary, JHEP Reports is dedicated to promoting scientific discoveries and innovations in liver diseases through the publication of high-quality research papers and reviews covering various aspects of hepatology.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


