法国原发性肝癌的“社会梯度”:一项全国性观察性研究
IF 7.5
1区 医学
Q1 GASTROENTEROLOGY & HEPATOLOGY
引用次数: 0
摘要
背景和目的社会剥夺与原发性肝癌(PLC)有关;然而,它对获得治愈性治疗和生存的影响仍不确定。我们评估了剥夺对医疗服务可及性的影响,并评估了护理集中是否可以改善国家层面的PLC管理。方法:我们使用法国国家出院数据库(2017-2021)进行了一项回顾性纵向队列研究,包括所有成年PLC患者。贫困是主要的暴露。主要和次要结局是获得根治性治疗(手术、移植或消融)和死亡率。采用随机效应logistic和Cox模型得出的调整优势比(aORs)和风险比(aHRs)对相关性进行评估,并由法国地区部门进行聚类。采用g计算来估计集中化(转诊医院内的治疗)对贫困患者获得治愈性治疗的绝对影响。结果62,351例患者(中位年龄[IQR], 71[63-78]岁,男性70.8%)中,45% (n = 27,872)被归为剥夺。剥夺与获得治愈性治疗的机会减少(aOR 0.89; 95% CI 0.85-0.92; p <0.001)和更高的死亡率(aHR 1.03; 95% CI 1.01-1.05; p <0.001)相关。在转诊医院治疗的患者中未观察到这些关联(aOR 1.03; 95% CI 0.98-1.09; aHR 1.02; 95% CI 0.98-1.06)。据估计,改善转诊医院的可及性可使获得治愈性治疗的可能性提高25% (95% CI 24-26),每年可能使811名贫困患者受益(范围730-895)。结论:在法国,剥夺原发性肝癌患者获得治愈性治疗的机会减少,死亡率增加。集中护理可以帮助缓解这些差异并改善结果。影响和意义已知社会剥夺会增加患原发性肝癌(PLC)的风险并降低生存率。然而,尚不清楚这是由于晚期诊断还是治疗机会有限,因为早期的研究主要考虑种族、民族、性别和保险状况等因素。我们的研究强调,在法国,被社会剥夺权利的PLC患者获得治愈性和姑息性治疗的机会减少,导致总体生存率降低。一个重要的发现是,社会剥夺的负面影响通过集中护理得到缓解——当病人在转诊中心诊断或治疗时,社会剥夺不再影响获得治愈性治疗或死亡率结果。这些发现支持在全国范围内采取集中的PLC管理策略,以改善社会经济弱势个体的护理结果。本文章由计算机程序翻译,如有差异,请以英文原文为准。
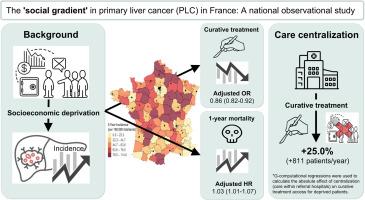
The ‘social gradient' in primary liver cancer in France: A national observational study
Background & Aims
Social deprivation has been associated with primary liver cancer (PLC); however, its impact on access to curative treatment and survival remains uncertain. We assessed the effect of deprivation on healthcare access and evaluated whether care centralization could improve PLC management at a national level.
Methods
We conducted a retrospective longitudinal cohort study using the French National Discharge Database (2017–2021), including all adult patients with PLC. Deprivation was the primary exposure. Primary and secondary outcomes were access to curative treatment (surgery, transplantation, or ablation) and mortality. Associations were assessed using adjusted odds ratios (aORs) and hazard ratios (aHRs) derived from random-effects logistic and Cox models, clustered by French regional departments. G-computation was applied to estimate the absolute effect of centralization (treatment within referral hospitals) on curative treatment access among deprived patients.
Results
Among 62,351 patients (median age [IQR], 71 [63–78] years; 70.8% male), 45% (n = 27,872) were classified as deprived. Deprivation was associated with reduced access to curative treatment (aOR 0.89; 95% CI 0.85–0.92; p <0.001) and higher mortality (aHR 1.03; 95% CI 1.01–1.05; p <0.001). These associations were not observed among patients treated in referral hospitals (aOR 1.03; 95% CI 0.98–1.09; aHR 1.02; 95% CI 0.98–1.06). Improving access to referral hospitals was estimated to increase the probability of receiving curative treatment by 25% (95% CI 24–26), potentially benefiting 811 deprived patients per year (range, 730–895).
Conclusions
Deprivation reduced access to curative treatment and increased mortality among patients with primary liver cancer in France. Care centralization could help mitigate these disparities and improve outcomes.
Impact and implications
Social deprivation is known to increase the risk of developing primary liver cancer (PLC) and to reduce survival. However, it has been unclear if this is due to late-stage diagnoses or limited access to treatments, as earlier studies mostly considered factors like race, ethnicity, sex, and insurance status. Our study highlighted that socially deprived patients with PLC in France face reduced access to curative and palliative treatments, resulting in lower overall survival rates. A key finding was that the negative impact of social deprivation was mitigated by care centralization – when patients were diagnosed or treated in referral centers, social deprivation no longer influenced access to curative treatments or mortality outcomes. These findings support the need for centralized PLC management strategies across the country to improve care outcomes for socioeconomically disadvantaged individuals.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

JHEP Reports
GASTROENTEROLOGY & HEPATOLOGY-
CiteScore
12.40
自引率
2.40%
发文量
161
审稿时长
36 days
期刊介绍:
JHEP Reports is an open access journal that is affiliated with the European Association for the Study of the Liver (EASL). It serves as a companion journal to the highly respected Journal of Hepatology.
The primary objective of JHEP Reports is to publish original papers and reviews that contribute to the advancement of knowledge in the field of liver diseases. The journal covers a wide range of topics, including basic, translational, and clinical research. It also focuses on global issues in hepatology, with particular emphasis on areas such as clinical trials, novel diagnostics, precision medicine and therapeutics, cancer research, cellular and molecular studies, artificial intelligence, microbiome research, epidemiology, and cutting-edge technologies.
In summary, JHEP Reports is dedicated to promoting scientific discoveries and innovations in liver diseases through the publication of high-quality research papers and reviews covering various aspects of hepatology.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


