睡眠特征与心血管疾病的发展轨迹。
IF 3.4
2区 医学
Q1 CLINICAL NEUROLOGY
引用次数: 0
摘要
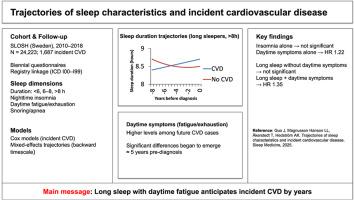
虽然睡眠特征与心血管疾病(CVD)有关,但大多数研究都集中在单个时间点或孤立的方面。更广泛的长期睡眠模式的预后价值尚不清楚。我们使用了瑞典纵向职业健康调查(SLOSH)中24223名参与者的数据,并在2010年至2018年期间进行了两年一次的随访。通过自我报告评估睡眠特征,并通过与国家登记的联系确定心血管事件结局。Cox比例风险模型估计了睡眠变量与心血管疾病之间的关联,混合效应模型评估了睡眠轨迹。在随访期间,1,687人出现心血管疾病。夜间失眠与CVD风险增加无关,除非伴有白天症状(HR 1.22, 95% CI 1.03-1.44;参考:没有失眠和白天症状)。同样,长时间睡眠(bbbb8小时)只有在伴有白天症状时才与较高的风险相关(HR 1.35, 95% CI 1.13-1.61;参考:6-8小时睡眠且无白天症状)。轨迹分析显示,基线时长时间睡眠的参与者后来发展为CVD,随着时间的推移,睡眠时间逐渐增加(CVD的β 8小时×时间= 0.06,95% CI 0.04-0.07; β ×时间2 = -0.005,95% CI -0.01至0.00),而没有CVD的长时间睡眠者表现出稳定或下降的模式。白天症状,特别是伴有睡眠时间延长或增加时,可能反映心血管疾病发生前的早期生理变化。这些发现强调了考虑睡眠模式及其随时间变化的重要性,而不仅仅是静态测量。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Trajectories of sleep characteristics and incident cardiovascular disease
While sleep characteristics have been associated with cardiovascular disease (CVD), most studies have focused on single timepoints or isolated aspects. The prognostic value of broader, long-term sleep patterns remains unclear.
We used data from 24,223 participants in the Swedish Longitudinal Occupational Survey of Health (SLOSH), with biennial follow-up between 2010 and 2018. Sleep characteristics were assessed via self-report and incident cardiovascular outcomes were identified through linkage to national registers. Cox proportional hazards models estimated associations between sleep variables and incident cardiovascular disease, and mixed-effects models assessed sleep trajectories.
During follow-up, 1,687 developed cardiovascular outcomes. Nighttime insomnia was not associated with increased CVD risk unless accompanied by daytime symptoms (HR 1.22, 95 % CI 1.03–1.44; reference: no insomnia and no daytime symptoms). Similarly, long sleep duration (>8 h) was associated with higher risk only when combined with daytime symptoms (HR 1.35, 95 % CI 1.13–1.61; reference: 6–8 h of sleep and no daytime symptoms). Trajectory analyses showed that participants with long sleep at baseline who later developed CVD had a gradual increase in sleep duration over time (β for CVD >8 h × time = 0.06, 95 % CI 0.04–0.07; β × time2 = −0.005, 95 % CI –0.01 to 0.00), while long sleepers who remained free of CVD showed stable or declining patterns.
Daytime symptoms, particularly when accompanied by prolonged or increasing sleep, may reflect early physiological changes preceding cardiovascular disease. These findings highlight the importance of considering sleep patterns and changes over time rather than static measures alone.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Sleep medicine
医学-临床神经学
CiteScore
8.40
自引率
6.20%
发文量
1060
审稿时长
49 days
期刊介绍:
Sleep Medicine aims to be a journal no one involved in clinical sleep medicine can do without.
A journal primarily focussing on the human aspects of sleep, integrating the various disciplines that are involved in sleep medicine: neurology, clinical neurophysiology, internal medicine (particularly pulmonology and cardiology), psychology, psychiatry, sleep technology, pediatrics, neurosurgery, otorhinolaryngology, and dentistry.
The journal publishes the following types of articles: Reviews (also intended as a way to bridge the gap between basic sleep research and clinical relevance); Original Research Articles; Full-length articles; Brief communications; Controversies; Case reports; Letters to the Editor; Journal search and commentaries; Book reviews; Meeting announcements; Listing of relevant organisations plus web sites.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


