在家庭环境中,睡眠中应用下相定向听觉刺激:一项连续七晚的可行性研究。
IF 3.4
2区 医学
Q1 CLINICAL NEUROLOGY
引用次数: 0
摘要
睡眠剥夺,也被称为“清醒疗法”,长期以来一直被认为是一种有效的抗抑郁药。相位定向听觉刺激(PTAS)被认为是一种吉祥的非侵入性夜间睡眠剥夺的替代品。特别是在慢波下行阶段伴随刺激呈现的Down-PTAS,可能通过选择性地减少慢波活动(SWA)而具有改善情绪的治疗潜力。由于ptas下降比睡眠剥夺更微妙,其影响可能会在多个晚上发展,因此有必要从睡眠实验室转移到家庭环境。因此,在本研究中,我们调查了在无人监督的家庭环境中用于下ptas的可穿戴设备的技术可行性、耐受性和潜在风险。方法:我们使用MHSL睡眠带版本3 (MHSL- sb)记录5名健康参与者(23.8±0.8岁,3名女性)连续7晚在家中使用(STIM)和不使用(SHAM)音调的额叶脑电图。在N2/N3睡眠期间,在慢波负峰之前不久,使用10秒交替的开关窗口传递音调。睡眠分期遵循美国睡眠医学学会(AASM)的指导方针。在67个可用的睡眠记录中,我们排除了3个由于参数调整,另外6个由于技术问题,留下58个睡眠记录(29个SHAM, 29个STIM)作进一步分析。低SWA (0.5-2 Hz, lSWA)在整个晚上、开-关窗口和睡眠周期中计算。时间-频率分析是在刺激开始时进行的。我们计算了将条件(STIM vs. SHAM)作为固定效应和随机参与者截距的线性混合效应模型。结果:87%的可用睡眠记录的数据质量足以用于分析,每个记录平均有超过1500个正确传递的刺激。Down-PTAS不影响睡眠结构,但它主要在睡眠压力和lSWA最高的第一个睡眠周期降低lSWA,特别是在OFF窗口。此外,刺激引起了类似k复合物的听觉诱发反应,这与先前的实验室发现一致。结论:我们的研究结果证明了down-PTAS在家庭环境中的成功实施,证实了其长期无监督使用的可行性。k复合物样听觉诱发反应可能掩盖了ON窗口期间lSWA的潜在减少,这对科学分析提出了挑战。综上所述,未来的临床研究现在应该评估下ptas对抑郁症患者的影响,在抑郁症患者中,减少lSWA可能部分模仿睡眠剥夺。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Application of down-phase targeted auditory stimulation during sleep in a home setting: A feasibility study across seven consecutive nights
Introduction
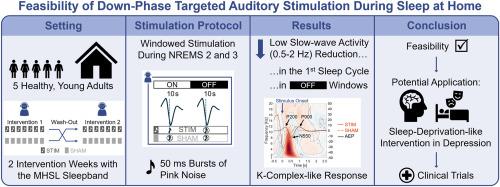
Sleep deprivation, also known as “wake therapy”, has long been recognized as a powerful antidepressant. Phase-targeted auditory stimulation (PTAS) has been suggested as an auspicious non-invasive nocturnal substitute for sleep deprivation. Down-PTAS with stimuli presentation during the down-phase of slow waves, in particular, may have therapeutic potential to improve mood by selectively reducing slow-wave activity (SWA). With down-PTAS being more nuanced than sleep deprivation, its effects presumably develop over multiple nights, thus necessitating transfer from sleep laboratory to home settings. Therefore, in this study, we investigated the technical feasibility, tolerability, and potential risks associated with a wearable device employed for down-PTAS in an unsupervised home setting.
Methods
We recorded frontal EEG using the MHSL Sleepband Version 3 (MHSL-SB) in five healthy participants (23.8 ± 0.8 years, three women) over seven consecutive nights with (STIM) and without (SHAM) tone application at their homes. Tones were delivered shortly before the negative peak of slow waves during N2/N3 sleep, using alternating 10-s ON-OFF windows. Sleep staging followed American Academy of Sleep Medicine (AASM) guidelines. Of the 67 available sleep recordings, we excluded three due to parameter adjustments and another six for technical issues, leaving 58 sleep recordings (29 SHAM, 29 STIM) for further analyses. Low SWA (0.5–2 Hz, lSWA) was computed across the entire night, ON-OFF windows, and sleep cycles. Time-frequency analyses were performed time-locked to stimulus onset. We computed linear mixed effect models with condition (STIM vs. SHAM) as a fixed effect and random participant intercepts.
Results
Data quality was sufficient for analyses in 87 % of the available sleep recordings, with an average of over 1500 correctly delivered stimuli per recording. Down-PTAS did not affect sleep architecture, but it reduced lSWA primarily during the first sleep cycle when sleep pressure and lSWA were highest, and particularly in OFF windows. Additionally, stimulation elicited a K-complex-like auditory evoked response, aligning with previous laboratory findings.
Conclusion
Our results demonstrate the successful implementation of down-PTAS in a home setting, confirming its feasibility for long-term, unsupervised use. The K-complex-like auditory evoked response may mask potential reductions in lSWA during ON windows, posing a scientific analytical challenge. Taken together, future clinical research should now assess the effects of down-PTAS in depressed patients, in whom reducing lSWA may partly mimic sleep deprivation.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Sleep medicine
医学-临床神经学
CiteScore
8.40
自引率
6.20%
发文量
1060
审稿时长
49 days
期刊介绍:
Sleep Medicine aims to be a journal no one involved in clinical sleep medicine can do without.
A journal primarily focussing on the human aspects of sleep, integrating the various disciplines that are involved in sleep medicine: neurology, clinical neurophysiology, internal medicine (particularly pulmonology and cardiology), psychology, psychiatry, sleep technology, pediatrics, neurosurgery, otorhinolaryngology, and dentistry.
The journal publishes the following types of articles: Reviews (also intended as a way to bridge the gap between basic sleep research and clinical relevance); Original Research Articles; Full-length articles; Brief communications; Controversies; Case reports; Letters to the Editor; Journal search and commentaries; Book reviews; Meeting announcements; Listing of relevant organisations plus web sites.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


