直肠癌直肠切除术后30天死亡率预测评分的开发和验证:国家癌症数据库分析。
IF 2.7
2区 医学
Q1 SURGERY
引用次数: 0
摘要
背景:本研究旨在探讨直肠癌手术后30天死亡率的预测因素,并利用显著的独立预测因子建立预测评分。方法:对2010-2017年国家癌症数据库进行回顾性病例对照分析。包括接受直肠切除术的I-III期直肠腺癌患者。将手术30天内死亡的患者与手术后30天存活的患者进行患者、疾病和治疗特征的比较。采用二元logistic回归建立预测模型;将30天死亡率的独立预测因子纳入预测风险评分,并使用国家癌症数据库(2018-2019)的另一个队列进行验证。结果:纳入53,651例直肠癌患者,其中男性占60.9%。30天死亡率为1.1%。30天死亡率的独立预测因子为年龄增加(优势比:1.07,95%可信区间:1.05-1.08)、男性(2.19,1.61-2.98)、黑人(2.16,1.44-3.25)、Charlson评分≥3(1.86,1.05-3.3)、肿瘤-淋巴结-转移期(1.66,1.12-2.46)、新辅助全身治疗(0.523,0.296-0.925)、住院时间延长(1.02,1.01-1.03)和转为开放手术(1.59,1.13-2.23)。开发了包含3个风险组的预测评分。三组间30天死亡率呈线性上升趋势(0.8% ~ 1.9% ~ 4.5%;P < 0.001)。在开发和验证数据集中,评分特异性分别为99.6%和99.5%,准确性分别为98.7%和98.8%。结论:将30天死亡率增加的独立预测因子纳入风险评分,其特异性和准确性超过98%。该评分可用于通过实施其他策略来降低短期死亡风险,从而改善高危患者的预后。本文章由计算机程序翻译,如有差异,请以英文原文为准。
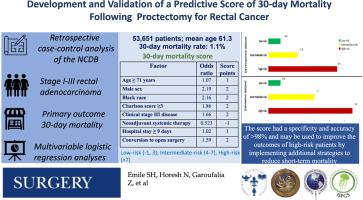
Development and validation of a predictive score of 30-day mortality following proctectomy for rectal cancer: A National Cancer Database analysis
Background
This study aimed to investigate predictors of 30-day mortality after rectal cancer surgery and develop a predictive score using significant independent predictors.
Methods
A retrospective case-control analysis of the National Cancer Database (2010–2017) was conducted. Patients with stage I-III rectal adenocarcinoma who underwent proctectomy were included. Patients who died within 30 days of surgery were compared to patients alive at 30 days after surgery for patient, disease, and treatment characteristics. Binary logistic regression was used to develop a predictive model; independent predictors of 30-day mortality were incorporated into a predictive risk score and validated using another cohort from the National Cancer Database (2018–2019).
Results
53,651 patients with rectal cancer (60.9% male) were included. Thirty-day mortality was 1.1%. Independent predictors of 30-day mortality were increased age (odds ratio: 1.07, 95% confidence interval: 1.05–1.08), male sex (2.19, 1.61–2.98), Black race (2.16, 1.44–3.25), Charlson score ≥3 (1.86, 1.05–3.3), tumor-node-metastasis stage III (1.66, 1.12–2.46), neoadjuvant systemic treatment (0.523, 0.296–0.925), prolonged hospitalization (1.02, 1.01–1.03), and conversion to open surgery (1.59, 1.13–2.23). A predictive score entailing 3 risk groups was developed. There was a linear trend of increased 30-day mortality across the three groups (0.8% to 1.9% to 4.5%; P < .001). Score specificity in the development and validation datasets was 99.6% and 99.5% and accuracy was 98.7% and 98.8%, respectively.
Conclusions
Independent predictors of increased 30-day mortality were incorporated into a risk score with a specificity and accuracy of more than 98%. The score may be used to improve outcomes of high-risk patients by implementing additional strategies to reduce the risk of short-term mortality.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Surgery
医学-外科
CiteScore
5.40
自引率
5.30%
发文量
687
审稿时长
64 days
期刊介绍:
For 66 years, Surgery has published practical, authoritative information about procedures, clinical advances, and major trends shaping general surgery. Each issue features original scientific contributions and clinical reports. Peer-reviewed articles cover topics in oncology, trauma, gastrointestinal, vascular, and transplantation surgery. The journal also publishes papers from the meetings of its sponsoring societies, the Society of University Surgeons, the Central Surgical Association, and the American Association of Endocrine Surgeons.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


