面临择期手术的成年患者精神困扰的患病率及其相关因素:一项横断面分析
IF 2.7
2区 医学
Q1 SURGERY
引用次数: 0
摘要
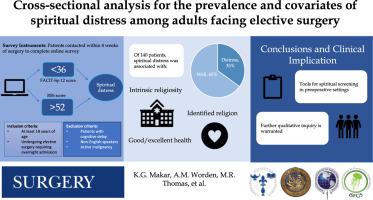
研究背景:晚期疾病的患者通常会经历精神上的痛苦,从而引发对生存的担忧。尽管外科手术的独特性,它唤起了主要的生活中断,精神困扰的流行在接受选择性手术的病人仍然未知。方法调查年龄≥18岁的择期手术患者,择期手术需住院4周。经验证的慢性疾病治疗功能评估-精神健康12(非疾病版)得分为36分,宗教和精神斗争量表得分为52分,表明精神痛苦。使用Pearson χ2、Welch 2-样本t检验和logistic回归来评估相关性。结果140例患者(有效率31%)中,49例精神痛苦(35%;慢性疾病治疗功能评估-精神健康平均[标准差]12.37[9],中位数[四分位数范围]宗教和精神斗争:5[9])。与没有痛苦的人相比,有痛苦的人内在宗教虔诚度得分显著降低(P < 0.001),组织和非组织宗教活动水平显著降低(P < 0.001)。抑郁(P < .001)、焦虑(P < .001)、未婚(P < .001)、经常财务担忧(P < .001)、健康状况一般/不佳(P < .001)和无宗教信仰(P < .001)与精神困扰有关。在调整分析中,内在的宗教信仰(优势比为0.71,95%可信区间为0.53-0.92,P = 0.013)、确定的宗教信仰(优势比为0.04,95%可信区间为0.00-0.57,P = 0.038)和良好/良好的健康状况(优势比为0.09,95%可信区间为0.01-0.39,P = 0.003)与较低的精神困扰发生率相关。结论超过三分之一的患者术前存在精神困扰,提示术前对精神护理的需求未得到满足。虽然手术遭遇是一个孤立的事件,但手术疾病患者会对健康、意义和目的产生严重的担忧。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Prevalence and correlates of spiritual distress in adult patients facing elective surgery: A cross-sectional analysis
Background
Patients with terminal disease, leading to existential concerns, commonly experience spiritual distress. Despite the uniqueness of the surgical encounter, which evokes major life disruption, the prevalence of spiritual distress in patients undergoing elective surgery remains unknown.
Methods
We surveyed patients ≥18 years of age scheduled within 4 weeks for elective surgery requiring overnight admission. Scores <36 on the validated Functional Assessment of Chronic Illness Therapy—Spiritual Well-being 12, Non-Illness Version or >52 on the Religious and Spiritual Struggles scale indicated spiritual distress. Pearson χ2, Welch 2-sample t tests, and logistic regression were used to evaluate associations.
Results
Of 140 patients (response rate 31%), 49 were spiritually distressed (35%; mean [standard deviation] Functional Assessment of Chronic Illness Therapy—Spiritual Well-being 12: 37 [9], median [interquartile range] Religious and Spiritual Struggles: 5 [13]). Those with distress had significantly lower intrinsic religiosity scores (P < .001) and lower levels of organizational and nonorganizational religious activity (P < .001 for both) than those without distress. Depression (P < .001), anxiety (P < .001), being unmarried (P < .001), frequent financial worry (P < .001), fair/poor health (P < .001), and no identified religion (P < .001) were associated with spiritual distress. On adjusted analysis, intrinsic religiosity (odds ratio, 0.71; 95% confidence interval, 0.53–0.92, P = .013), identified religion (odds ratio, 0.04; 95% confidence interval, 0.00–0.57; P = .038), and good/excellent health (odds ratio, 0.09; 95% confidence interval, 0.01–0.39; P = .003) were associated with lower odds of spiritual distress.
Conclusion
More than one-third of patients experienced spiritual distress preoperatively, suggesting an unmet need to facilitate spiritual care in the preoperative period. Although the surgical encounter is an isolated event, patients with surgical disease navigate serious concerns related to health, meaning, and purpose.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Surgery
医学-外科
CiteScore
5.40
自引率
5.30%
发文量
687
审稿时长
64 days
期刊介绍:
For 66 years, Surgery has published practical, authoritative information about procedures, clinical advances, and major trends shaping general surgery. Each issue features original scientific contributions and clinical reports. Peer-reviewed articles cover topics in oncology, trauma, gastrointestinal, vascular, and transplantation surgery. The journal also publishes papers from the meetings of its sponsoring societies, the Society of University Surgeons, the Central Surgical Association, and the American Association of Endocrine Surgeons.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


