冠状动脉钙负荷的合并队列方程与美国心脏协会预防风险计算器
IF 5.9
Q1 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
摘要
合并队列方程(PCE)和心血管疾病事件预测风险计算器(prevention)评估动脉粥样硬化性心血管疾病(ASCVD)的风险。冠状动脉钙(CAC)评分比传统的危险因素更能增强ASCVD的风险分层,但PCE和prevention风险组的CAC负担仍不清楚。本研究评估了CAC负担在PCE和prevention风险组中的分布。方法回顾性队列研究纳入7610例2010 - 2023年间接受临床指示CAC评分的无症状患者。使用PCE和PREVENT计算10年ASCVD风险(低5 %,中边缘5 % - 19 %,高≥20%)。使用Kendall Tau测试比较不同风险组的CAC评分(0、1-99、100-299、≥300)。结果患者平均年龄57±9岁;41%的患者是女性,11%是黑人。PCE和PREVENT分别将52.5%和72.6%归为低危,41%和27.1%归为中危,6.5%和3.7%归为高危。PCE/ prevention风险较高的组中位CAC升高(p < 0.001)。对于临界-中危患者,71%的PCE患者和79%的PREVENT患者的CAC>;0,而对于低危患者,CAC>;0分别为45%和51%。在临界危险组(5 - 7.5%)中,20.7%的PCE和35%的ASCVD PREVENT组的cac100。结论在预防和PCE的低危分层组中均有大量患者存在非零CAC,而在预防和PCE的交界-中间分层组中,CAC的分布具有异质性,这些结果强调了CAC在PCE和预防之外的进一步分层风险中的重要性。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Coronary artery calcium burden across the pooled cohort equation versus the American Heart Association PREVENT risk calculator
Background
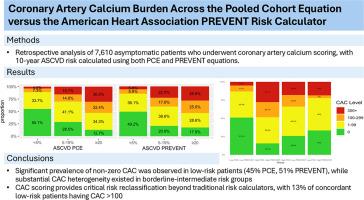
The Pooled Cohort Equation (PCE) and the Predicting Risk of cardiovascular disease EVENTs (PREVENT) calculator assess atherosclerotic cardiovascular disease (ASCVD) risk. Coronary artery calcium (CAC) scoring enhances ASCVD risk stratification beyond traditional risk factors, but CAC burden across PCE versus PREVENT risk groups remains unclear. This study evaluates the distribution of CAC burden across PCE and PREVENT risk groups.
Methods
A retrospective cohort study was conducted involving 7610 asymptomatic patients who underwent clinically indicated CAC scoring between 2010 and 2023. Ten-year ASCVD risk was calculated using PCE and PREVENT (low<5, borderline-intermediate 5–19, high≥20 %). CAC scores (0, 1–99, 100–299, ≥300) were compared across risk groups using Kendall Tau tests.
Results
The mean age was 57±9 years; 41 % of patients were women and 11 % identified as Black. PCE and PREVENT classified 52.5 % and 72.6 % as low-risk, 41 % and 27.1 % as borderline-intermediate risk, and 6.5 % and 3.7 % as high-risk, respectively. Higher PCE/PREVENT risk groups had increased median CAC (p < 0.001). For borderline-intermediate risk, 71 % for PCE and 79 % for PREVENT had CAC>0, while for low risk, 45 % and 51 %. Within the borderline risk group (5–7.5 %), 20.7 % of PCE and 35 % of ASCVD PREVENT group had CAC>100.
Conclusions
A significant number of patients had non-zero CAC in low-risk stratification groups for both PREVENT and PCE. CAC distribution was heterogeneous in the borderline-intermediate groups for both PREVENT and PCE. These results emphasize the significance of CAC in further stratifying risk beyond the PCE and PREVENT.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

American journal of preventive cardiology
Cardiology and Cardiovascular Medicine
CiteScore
6.60
自引率
0.00%
发文量
0
审稿时长
76 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


