早期血栓形成前评估在左心耳关闭后器械相关血栓风险分层中的作用
IF 2.8
Q3 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
摘要
背景左心房附件关闭术(LAAC)越来越多地用于预防非瓣膜性心房颤动和口服抗凝禁忌症患者的脑卒中。LAAC术后早期血栓前状态评估在评估器械相关血栓(DRT)风险中的潜在作用尚不清楚。方法纳入147例有口服抗凝禁忌症的LAAC患者。凝血激活标志物-凝血酶原片段1 + 2和凝血酶抗凝血酶iii -在基线和术后7天测量。根据delta(%)变化的第50个百分位数,将患者分为低或高血栓前状态。评估特定的δ %阈值,可以作为排除DRT的非侵入性截止值。结果53例(36.1%)患者被归为高血栓前状态。DRT发生在9例患者中(6.1%),其中高血栓原组的发生率明显更高(15.1比1.1%,p < 0.001)。多变量分析发现laac后凝血激活标志物升高是DRT的独立预测因子(校正优势比:13.84 [1.65-115.89],p = 0.015)。建议的凝血酶原片段1 + 2(74.11%)和凝血酶抗凝血酶III(120.74%)阈值为98.9%的阴性预测值。使用这些阈值,75.5%的患者被归为DRT低风险。在随访中,低风险和高风险DRT组之间没有观察到临床差异。结论早期评价凝血指标对LAAC术后DRT风险有重要意义。所提出的阈值具有很高的阴性预测值,可有效识别DRT风险低的患者,并支持将其作为非侵入性工具安全地排除DRT。这些标记物可以实现早期抗血栓降级,减少重复成像的需要。进一步的研究是必要的。本文章由计算机程序翻译,如有差异,请以英文原文为准。
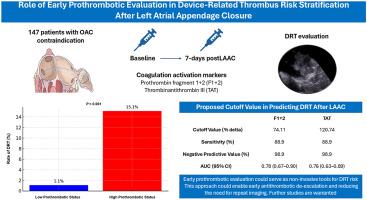
Role of Early Prothrombotic Evaluation in Device-Related Thrombus Risk Stratification After Left Atrial Appendage Closure
Background
Left atrial appendage closure (LAAC) is increasingly used for stroke prevention in patients with non-valvular atrial fibrillation and contraindications to oral anticoagulation. The potential role of early prothrombotic status assessment in evaluating device-related thrombus (DRT) risk following LAAC remains unclear.
Methods
The study included 147 patients undergoing LAAC with oral anticoagulation contraindication. Coagulation activation markers—prothrombin fragment 1 + 2 and thrombin antithrombin III—were measured at baseline and 7 days postprocedure. Based on the 50th percentile of delta (%) changes, patients were classified into low or high prothrombotic status. Specific delta % thresholds were assessed, which could serve as noninvasive cutoffs to rule out DRT.
Results
A total of 53 patients (36.1%) were classified as having high prothrombotic status. DRT occurred in 9 patients (6.1%), with a significantly higher incidence in the high prothrombotic group (15.1 vs. 1.1%, p < 0.001). Multivariable analysis identified elevated post-LAAC coagulation activation markers as independent predictors of DRT (adjusted odds ratio: 13.84 [1.65-115.89], p = 0.015). Proposed thresholds for prothrombin fragment 1 + 2 (74.11%) and thrombin antithrombin III (120.74%) demonstrated negative predictive values of 98.9%. Using these thresholds, 75.5% of patients were classified as low risk for DRT. No clinical differences were observed at follow-up between the low- and high-risk DRT groups.
Conclusions
Early evaluation of coagulation markers provides valuable insight into DRT risk after LAAC. The proposed thresholds demonstrate a high negative predictive value, effectively identifying patients at low risk for DRT and supporting their use as noninvasive tools to safely rule out DRT. These markers could enable early antithrombotic de-escalation and reduce the need for repeat imaging. Further studies are warranted.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Structural Heart
Medicine-Cardiology and Cardiovascular Medicine
CiteScore
1.60
自引率
0.00%
发文量
81
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


