不同睡眠特征对长期骨骼肌损失的影响:一项队列研究
IF 3.6
2区 医学
Q2 GERIATRICS & GERONTOLOGY
引用次数: 0
摘要
目的:睡眠不足可能导致激素失衡、肥胖增加和能量代谢紊乱。这项研究旨在阐明睡眠特征对骨骼肌质量损失的长期影响。方法我们分析了421,688名参与者(男性220,902名,女性200786名,平均年龄39.1±10.2岁)的数据,这些参与者在基线时骨骼肌指数不高。使用匹兹堡睡眠质量指数评估睡眠质量。使用生物电阻抗分析估计骨骼肌质量。低骨骼肌指数是由2019年亚洲肌肉减少症工作组共识诊断的。协变量包括人口统计学特征、健康行为、生活方式相关因素、合并症、生化指标和饮食摄入。采用多变量Cox回归分析评估睡眠特征对低骨骼肌指数发生率的影响。结果骨骼肌指数低的参与者整体睡眠质量较差。值得注意的是,骨骼肌指数、体脂量、内脏脂肪面积和体脂百分比都与睡眠质量有显著差异。生化评估显示血清蛋白、葡萄糖代谢标志物、脂质谱、肾脏和肝脏功能以及炎症标志物与睡眠质量有显著差异。在调整混杂因素后,较长的睡眠潜伏期和较低的睡眠效率仍然是低骨骼肌指数的重要因素。此外,频繁使用睡眠药物和严重的睡眠障碍与低骨骼肌指数显著相关。结论睡眠质量差,尤其是睡眠潜伏期长、睡眠效率低、频繁使用睡眠药物和严重的睡眠障碍,严重影响骨骼肌质量的维持。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Impact of diverse sleep characteristics on long-term skeletal muscle loss: A cohort study
Objective
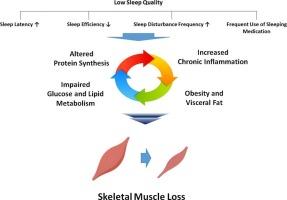
Poor sleep may contribute to hormonal imbalance, increased adiposity, and disruption of energy metabolism. This study aimed to clarify the long-term impact of sleep characteristics on loss of skeletal muscle mass.
Methods
We analyzed data from 421,688 participants (220,902 males, 200786 females; mean age 39.1 ± 10.2 years) without a low skeletal muscle index at baseline. Sleep quality was assessed using the Pittsburgh Sleep Quality Index. Skeletal muscle mass was estimated using bioelectrical impedance analysis. Low skeletal muscle index was diagnosed by the Asian Working Group for Sarcopenia 2019 Consensus. Covariates included demographic characteristics, health behavior, and lifestyle-related factors, comorbidities, biochemical markers, and dietary intake. Multivariate Cox regression analyses were conducted to assess effects of sleep characteristics on incidence of low skeletal muscle index.
Results
Participants who developed low skeletal muscle index exhibited poorer general sleep quality. Notably, skeletal muscle index, body fat mass, visceral fat area, and body fat percentage all significantly differed with sleep quality. Biochemical assessment revealed significant variations in serum proteins, glucose metabolism markers, lipid profiles, kidney and liver function, and inflammatory markers with sleep quality. After adjusting for confounders, longer sleep latency and lower sleep efficiency remained significant contributors to low skeletal muscle index. Additionally, frequent use of sleep medication and severe sleep disturbances were significantly associated with low skeletal muscle index.
Conclusion
Poor sleep quality, particularly longer sleep latency, lower sleep efficiency, frequent use of sleep medication and severe sleep disturbance, significantly impacts maintenance of skeletal muscle mass.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Maturitas
医学-妇产科学
CiteScore
9.10
自引率
2.00%
发文量
142
审稿时长
40 days
期刊介绍:
Maturitas is an international multidisciplinary peer reviewed scientific journal of midlife health and beyond publishing original research, reviews, consensus statements and guidelines, and mini-reviews. The journal provides a forum for all aspects of postreproductive health in both genders ranging from basic science to health and social care.
Topic areas include:• Aging• Alternative and Complementary medicines• Arthritis and Bone Health• Cancer• Cardiovascular Health• Cognitive and Physical Functioning• Epidemiology, health and social care• Gynecology/ Reproductive Endocrinology• Nutrition/ Obesity Diabetes/ Metabolic Syndrome• Menopause, Ovarian Aging• Mental Health• Pharmacology• Sexuality• Quality of Life
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


