在老年人中,程序性学习随着OSA的严重程度而恶化,并且对短时间暴露的补充氧治疗不敏感
IF 3.4
2区 医学
Q1 CLINICAL NEUROLOGY
引用次数: 0
摘要
研究目的阻塞性睡眠呼吸暂停(OSA)与中青年认知缺陷有关,但对老年人认知能力的影响尚不清楚,老年人与年龄相关的认知能力下降的风险更大。我们研究了OSA严重程度如何影响老年人的认知表现,以及短时间暴露于补充氧气是否可以改变这种关系,同时也利用病理生理学来确定氧气治疗的候选对象。方法从圣地亚哥社区招募65名目前未接受OSA治疗的参与者(65岁以上),其中大多数表现为中度或重度OSA。参与者按随机顺序在室内空气或夜间补氧(NOS)条件下进行了两晚的实验室多导睡眠描记。参与者在睡觉前和睡觉后都进行了睡眠依赖性认知测试。结果NOS治疗可减轻夜间低氧血症。在整个样本中,呼吸暂停低通气事件(AHI)的频率没有降低,但我们发现,在OSA严重程度为15次/小时或咽萎性低于中位数的参与者中,对AHI有显著的治疗效果。运动序列任务改善与夜间AHI呈负相关,但在整个样本或反应亚组中,NOS治疗并没有改善夜间表现。结论与年轻人相比,老年人睡眠呼吸暂停越严重,其运动程序学习能力越差。然而,一晚NOS治疗对程序性学习没有影响,这表明osa相关的认知缺陷是由睡眠中断和缺氧的慢性影响引起的。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Procedural learning worsens with OSA severity in older adults and is insensitive to short exposure supplemental oxygen therapy
Study objectives
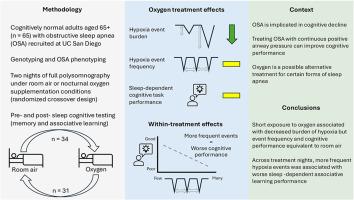
Obstructive sleep apnea (OSA) has been associated with cognitive deficiencies in young and middle aged adults but the impact on cognition in older adults, who are at greater risk of age-related cognitive decline, is less well understood. We investigated how OSA severity impacts cognitive performance in older adults and whether short exposure to supplemental oxygen can modify this relationship, whilst also leveraging pathophysiology to identify oxygen treatment candidates.
Methods
65 participants (65+ years) not currently receiving OSA treatment were recruited from the San Diego community, most of whom presented with moderate or severe OSA. Participants undertook two nights of in-laboratory polysomnography under room air or nocturnal oxygen supplementation (NOS) conditions in randomized order. Participants performed sleep-dependent cognitive tests both before and after sleep.
Results
Nocturnal hypoxemia was reduced with NOS treatment. There was no reduction in the frequency of apnea-hypopnea events (AHI) in the full sample, however we found a significant treatment effect on AHI among participants with OSA severity >15 events/hour or among those with below-median pharyngeal collapsibility. Motor sequence task improvement was negatively correlated with AHI within a night but NOS treatment did not improve performance between nights in either the full sample or a responsive sub-group.
Conclusions
As in younger adults, more severe sleep apnea is associated with worse motor procedural learning in older adults. However, a single night of NOS treatment had no effect on procedural learning, suggesting that OSA-related cognitive deficits result from chronic impacts of sleep disruption and hypoxia.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Sleep medicine
医学-临床神经学
CiteScore
8.40
自引率
6.20%
发文量
1060
审稿时长
49 days
期刊介绍:
Sleep Medicine aims to be a journal no one involved in clinical sleep medicine can do without.
A journal primarily focussing on the human aspects of sleep, integrating the various disciplines that are involved in sleep medicine: neurology, clinical neurophysiology, internal medicine (particularly pulmonology and cardiology), psychology, psychiatry, sleep technology, pediatrics, neurosurgery, otorhinolaryngology, and dentistry.
The journal publishes the following types of articles: Reviews (also intended as a way to bridge the gap between basic sleep research and clinical relevance); Original Research Articles; Full-length articles; Brief communications; Controversies; Case reports; Letters to the Editor; Journal search and commentaries; Book reviews; Meeting announcements; Listing of relevant organisations plus web sites.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


