主动脉瓣狭窄的长期预后:一组选定患者的死亡率分析。
摘要
背景:主动脉瓣狭窄(Aortic stenosis, AS)是一种常见的获得性心脏瓣膜疾病,发病率越来越高,尤其是在老年人中。AS的表现、合并症和结果的性别差异仍未得到充分探讨,需要进一步研究以优化个性化治疗策略。目的:评估AS患者的临床和人口学特征、合并症和生存结果,按性别和主动脉瓣形态分层。方法:回顾性分析联邦国家预算机构“va Almazov国家医学研究中心”2009-2018年145,454例超声心动图检查,确定84,851例符合纳入标准(Vmax≥2.0 m/s,年龄≥18岁)的患者。患者按性别和瓣膜形态进行分层(二尖瓣主动脉瓣[BAV] vs三尖瓣主动脉瓣[TAV])。采用Kaplan-Meier分析对475例AS患者在16年期间(2009-2025年)的生存率进行了评估。统计比较使用STATISTICA v. 10.0, p值来源于p检验。结果:在队列中,4998名男性和6322名女性患有AS。AS患者年龄较大(中位年龄64岁vs. 57岁,p < 0.0001),收缩压高于非AS患者(140 mmHg vs. 130 mmHg, p < 0.0001)。AS女性患者年龄也较大(中位年龄为70岁vs. 58岁,p < 0.0001),收缩压(140 vs. 130 mmHg, p < 0.0001)和舒张压(80 vs. 80 mmHg, p < 0.0001)较高。男性AS患者高脂血症(HLP)发生率较高(26.3% vs. 10.3%, p < 0.0001),而女性AS患者冠状动脉疾病(CAD)发生率较高(35.7% vs. 26.4%, p < 0.0001),糖尿病(DM)发生率较高(13.4% vs. 10.2%, p < 0.0001),肥胖发生率较高(10.9% vs. 10.2%, p = 0.06)。慢性心力衰竭(CHF)在AS患者中更常见,无论性别,与无AS患者相比(男性53.4%对41.8%,p < 0.0001;女性54.5%对37.5%,p < 0.0001)。BAV与较高的AS患病率相关(男性54.5%,女性66.4%)。生存分析显示死亡率更高。在16年的随访期间,死亡率为21.7%。结论:在一个有代表性的AS队列中,死亡率达到21.7%,强调了该疾病的进行性及其长期影响。年龄超过68.5岁、存在主动脉反流(AR)、主动脉喷流峰值速度增加和最大主动脉直径增大对生存率有负面影响。主动脉瓣置换术对患者存活率的影响并不显著。在不同程度的主动脉AS严重程度的患者中,β受体阻滞剂治疗不仅证明了其安全性,而且在降低死亡率(提高生存率)方面也显示出积极的作用。相比之下,血管紧张素II受体阻滞剂(ARBs)与钙通道阻滞剂(CCBs)联合使用对AS患者非常危险,并降低其生存率。主动脉瓣置换术对患者存活率的影响并不显著。相反,缺乏纤溶治疗和抗凝治疗与预后改善有关。相反,抗心律失常药物和他汀类药物的施用与提高生存结果相关,可能归因于它们对共存的合并症的影响。需要进一步的研究来描述它们的确切机制和贡献。这些结果强调了早期识别、全面风险评估和个性化管理策略对改善AS患者预后的重要性。
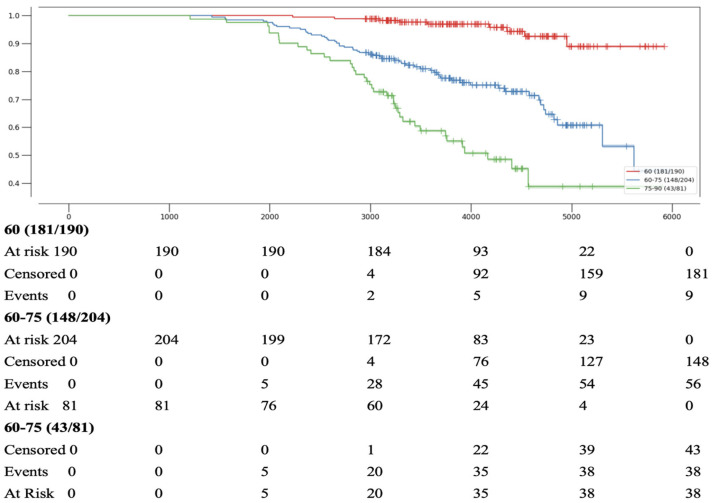
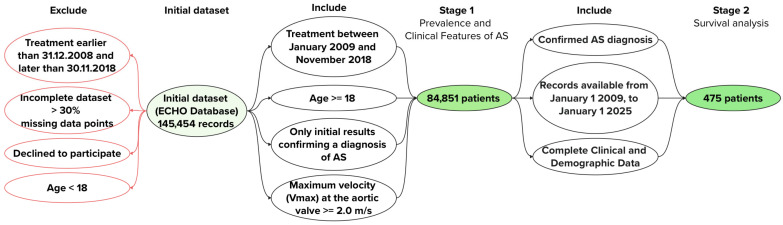
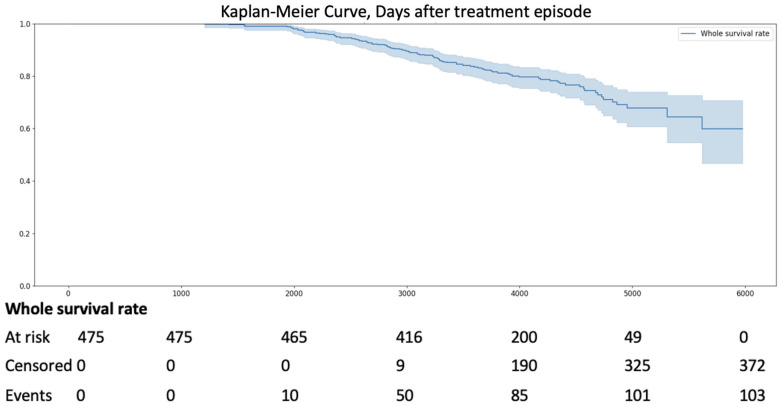
Background: Aortic stenosis (AS) is a prevalent acquired heart valve disease with increasing incidence, particularly among older adults. Gender-specific differences in AS presentation, comorbidities, and outcomes remain underexplored, necessitating further investigation to optimize personalized treatment strategies. Objective: To evaluate the clinical and demographic characteristics, comorbidities, and survival outcomes of patients with AS, stratified by gender and aortic valve morphology. Methods: A retrospective analysis of 145,454 echocardiographic examinations (2009-2018) at the Federal State Budgetary Institution "V.A. Almazov National Medical Research Centre" identified 84,851 patients meeting the inclusion criteria (Vmax ≥ 2.0 m/s, age ≥ 18 years). Patients were stratified by gender and valve morphology (bicuspid aortic valve [BAV] vs. tricuspid aortic valve [TAV]). Survival was assessed in 475 pts with AS over a 16-year period (2009-2025) using Kaplan-Meier analysis. Statistical comparisons utilized STATISTICA v. 10.0, with p-values derived from P-tests. Results: Of the cohort, 4998 men and 6322 women had AS. Men with AS were older (median 64 vs. 57 years, p < 0.0001) and had higher systolic blood pressure (140 vs. 130 mmHg, p < 0.0001) than men without AS. Women with AS were also older (median 70 vs. 58 years, p < 0.0001) with higher systolic (140 vs. 130 mmHg, p < 0.0001) and diastolic blood pressure (80 vs. 80 mmHg, p < 0.0001). Men with AS had higher rates of hyperlipidemia (HLP) (26.3% vs. 10.3%, p < 0.0001), while women with AS had increased coronary artery disease (CAD) (35.7% vs. 26.4%, p < 0.0001), diabetes mellitus (DM) (13.4% vs. 10.2%, p < 0.0001), and obesity (10.9% vs. 10.2%, p = 0.06). Chronic heart failure (CHF) was more frequently reported in patients with AS, regardless of gender, compared to patients without AS (in men 53.4% vs. 41.8%, p < 0.0001; in women 54.5% vs. 37.5%, p < 0.0001). BAV was associated with higher AS prevalence (54.5% in men, 66.4% in women). Survival analysis revealed higher mortality. Over the 16-year follow-up period, the mortality rate was 21.7%. Conclusions: Mortality in a representative AS cohort reached 21.7%, underscoring the progressive nature of the disease and its long-term impact. Survival was negatively affected by age over 68.5 years, as well as the presence of aortic regurgitation (AR), increased peak aortic jet velocity, and enlarged maximum aortic diameter. Aortic valve replacement demonstrates an insignificant effect on patient survival rates. Beta-blocker therapy in patients with varying degrees of aortic AS severity has not only demonstrated its safety but has also shown a positive effect on reducing mortality (improving survival). In contrast, the combination of angiotensin II receptor blockers (ARBs) with calcium channel blockers (CCBs) is quite dangerous for patients with AS and reduces their survival. Aortic valve replacement demonstrates an insignificant effect on patient survival rates. In contrast, the absence of fibrinolytic therapy and anticoagulant treatment is associated with an improved prognosis. Conversely, the administration of antiarrhythmic agents and statins is correlated with enhanced survival outcomes, potentially attributable to their influence on coexisting comorbidities. Further research is required to delineate their precise mechanisms and contributions. These results emphasize the importance of early identification, comprehensive risk assessment, and individualized management strategies in improving outcomes for patients with AS.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


