报道尼日利亚首个微创脊柱手术系列:一项描述性单中心回顾性队列研究。
摘要
微创脊柱手术(MISS)自从引入脊柱外科以来,获得了越来越多的关注,其结果比传统的开放方法更好。它最近才被引入尼日利亚,在那里很少表演。为了改善在他的祖国获得最先进的神经外科服务的机会,这位资深作者在美国实施了MISS,并于2017年开始在尼日利亚实施。我们的目标是描述我们在尼日利亚的MISS手术经验,尼日利亚是一个高贫困指数的中低收入国家(LMIC),并报告该国的第一批此类手术。这是一项描述性单中心回顾性队列研究,通过对我们数据库中2017年4月至2022年5月期间胸、腰椎和腰骶脊柱区域因退行性椎间盘疾病而发生MISS的患者进行回顾。检索并分析人口统计学、围手术期参数(手术时间[SDn]、估计失血量[EBL]、住院时间[LOS])、围手术期手术部位并发症和患者报告的预后(数值评定量表[NRS]和Oswestry残疾指数[ODI])数据。患者报告结果(PROs)的最小重要差异(MID)定义为NRS的2点变化和ODI的5.9-20点差异的改善。同一位主刀医师以相似的手术技术和围手术期处理进行手术。143例患者资料非正态分布。年龄中位数为62岁,男性占55.9%。51%的患者行微创(MIS)椎板切除术;45.5%和3.5%分别行mis -经椎间孔腰椎椎间融合术(TLIF)和mis -显微椎间盘切除术。大多数(73.4%)发生在腰椎,25.2%发生在腰骶交界处,1.4%发生在胸椎。中位SDn、EBL和LOS分别为112分钟、50毫升和3天。围手术期手术部位并发症发生率为4.9%。在基线和一年随访期间,PROs和MID均有统计学改善。本研究的围手术期参数和手术部位并发症发生率与先前在高收入国家对MIS腰椎减压(椎板切除术和微椎间盘切除术)和MIS- tlif的研究结果相当。此外,患者在PROs方面的改善与高收入国家的脊柱外科研究结果相当。我们努力将MISS作为我们在尼日利亚实践的一部分,这是由于需要在有能力的中低收入国家部署、发展和维持有益的尖端护理,同时不忽视“储备”程序。MISS在尼日利亚是可行的,在我们的实践中,它的特点是令人满意的围手术期参数,围手术期手术部位并发症发生率,以及与MISS和其他高收入国家进行的脊柱手术相媲美的PROs,在这些国家MISS很普遍。
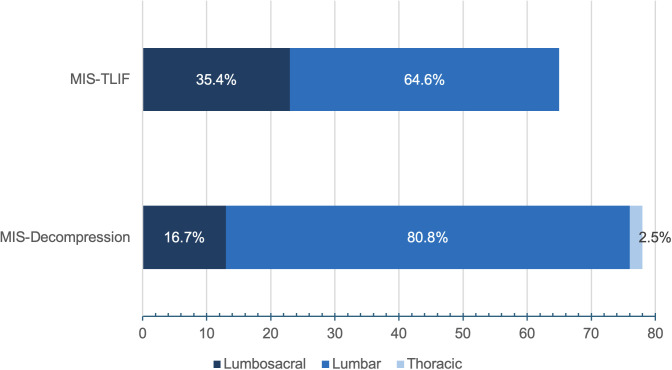
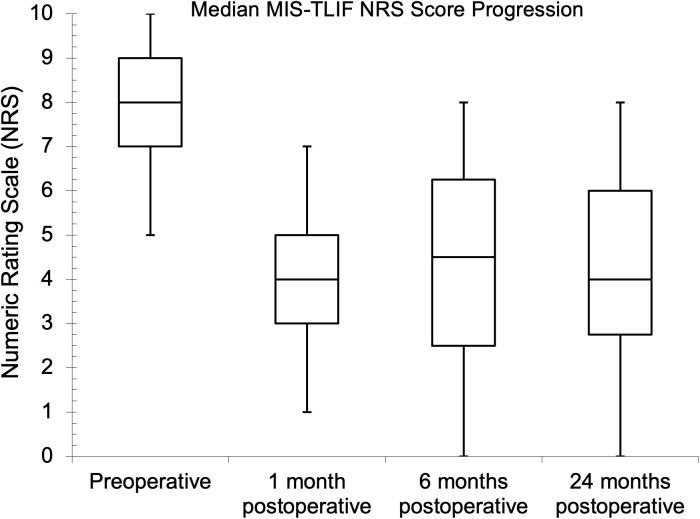
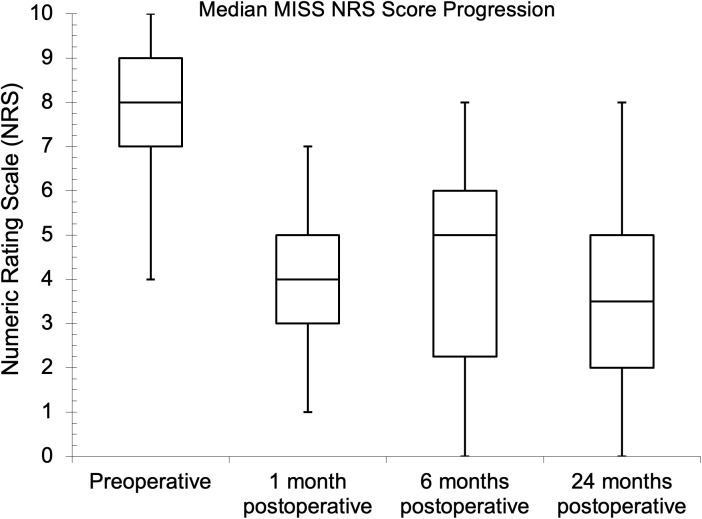
Minimally invasive spine surgery (MISS) has gained traction since its introduction into the spine surgery armamentarium, resulting in better outcomes than the traditional open approaches. It was only recently introduced in Nigeria, where it is rarely performed. In a bid to improve access to state-of-the-art neurosurgical services in his home country, the senior author, having practiced MISS in the United States, started performing it in Nigeria in 2017. We aim to describe our MISS experience in Nigeria, a lower-middle-income country (LMIC) with high poverty indices, and report the first series of these surgeries in the country. This is a descriptive single-center retrospective cohort study performed through a review of our database of patients who had MISS for degenerative disc disease involving the thoracic, lumbar, and lumbosacral spine regions from April 2017 to May 2022. Demographic, perioperative parameter (surgery duration [SDn], estimated blood loss [EBL], length of hospital stay [LOS]), perioperative surgical site complication, and patient-reported outcome (Numeric Rating Scale [NRS] and Oswestry Disability Index [ODI]) data were retrieved and analyzed. Minimal important differences (MID) in the patient-reported outcomes (PROs) were defined as improvements of a two-point change for NRS and a 5.9-20-point difference for ODI. The same lead surgeon performed the procedures with similar operative techniques and perioperative management. The data of the 143 patients were not normally distributed. The median age was 62 years, and males comprised 55.9%. Fifty-one percent of the patients had minimally invasive (MIS) laminectomy; 45.5% and 3.5% had MIS-transforaminal lumbar interbody fusion (TLIF) and MIS-microdiscectomy, respectively. Most (73.4%) were in the lumbar spine, 25.2% involved the lumbosacral junction, and 1.4% were in the thoracic spine. Median SDn, EBL, and LOS were 112 mins, 50 mL, and 3 days, respectively. The perioperative surgical site complication rate was 4.9%. The PROs showed statistical improvement and MID between baseline and one-year follow-up. This study's perioperative parameters and surgical site complication rates are comparable to those obtained from previous work on MIS lumbar decompression (laminectomy and microdiscectomy) and MIS-TLIF in higher-income countries. Additionally, the patients' improvements in the PROs were comparable to findings in spine surgery research in higher-income countries. Our efforts to introduce MISS as part of our practice in Nigeria are informed by the need for deploying, developing, and maintaining beneficial cutting-edge care in LMICs where the capacity exists, while not neglecting the 'stock' procedures. MISS is available in Nigeria, and it is characterized in our practice by satisfactory perioperative parameters, perioperative surgical site complication rates, and PROs that are comparable with those obtained from MISS and other spine surgeries performed in countries with high incomes, where MISS is rife.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


