丹麦心肌梗死患者的护理途径——保健和药物利用
IF 2.5
Q2 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
摘要
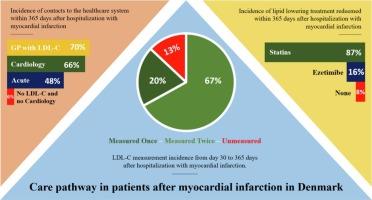
背景:心肌梗死(MI)后,建议患者降低低密度脂质胆固醇(LDL-C)水平,并进行心脏康复以防止复发。尽管降低心肌梗死后LDL-C至关重要,但许多患者未能达到足够的水平,导致心血管事件复发。因此,该研究的目的是调查心肌梗死一年后的随访和降脂治疗的使用情况。方法:这项基于登记的丹麦全国观察性研究纳入了2018年至2021年所有住院的心肌梗死患者。出院后对患者进行为期一年的LDL-C测量、与不同医护人员的接触以及降脂治疗。结果共纳入24977例患者。在随访期间,检测一次和两次LDL-C的发生率分别为87%和67%。就诊心内科、全科医生进行LDL-C检测和急诊就诊的患者分别为66%、70%和48%。大多数患者至少一次(87%)或两次(82%)使用他汀类药物进行治疗,而依折麦比(16%)和其他药物的使用频率较低。住院时LDL-C≥1.4 mmol/L的年轻、高学历、合并症较少的男性在心肌梗死后更有可能接受LDL-C测量随访或前往心内科就诊。这些发现表明,很大一部分患者在心肌梗死一年后没有接受降脂治疗或没有按照指南进行监测。这表明需要进一步监测心肌梗死患者的LDL-C水平和就诊情况。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Care pathway in patients after myocardial infarction in Denmark − healthcare and drug utilization
Background
Following myocardial infarction (MI), patients are recommended to lower their low-density lipid cholesterol (LDL-C) levels and undergo cardiac rehabilitation to prevent recurrent events. Although lowering LDL-C is vital post-MI, many patients fail reaching sufficient levels, resulting in recurrent cardiovascular events. The aim of the study was therefore to investigate the follow-up and the utilisation of lipid lowering therapy one year after MI.
Methods
This register-based nationwide Danish observational study included all hospitalized patients with an incident MI from 2018 to 2021, discharged alive. Patients were followed for one year after discharge with respect to LDL-C measurements, contacts with different healthcare actors, and lipid lowering therapy.
Results
A total of 24,977 patients were included. During follow-up, the incidence of having an LDL-C measured once and twice were 87 % and 67 %, respectively. The incidence of patients visiting a cardiology department, general practitioner with an LDL-C measurement, and having an acute hospital contact were 66 %, 70 %, and 48 %. Statin therapy was redeemed by most patients at least once (87 %) or twice (82 %), while ezetimibe (16 %) and other drugs were prescribed less frequently. Younger, higher educated, less comorbid males with LDL-C ≥ 1.4 mmol/L at hospitalization were more likely to be followed-up with LDL-C measurement or visit to a cardiology department post-MI.
Conclusion
These findings show that a large proportion of patients are not receiving lipid lowering therapy or are not monitored according to guidelines one year after an MI. This suggests a further need for monitoring MI patients with LDL-C levels and healthcare visits.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

IJC Heart and Vasculature
Medicine-Cardiology and Cardiovascular Medicine
CiteScore
4.90
自引率
10.30%
发文量
216
审稿时长
56 days
期刊介绍:
IJC Heart & Vasculature is an online-only, open-access journal dedicated to publishing original articles and reviews (also Editorials and Letters to the Editor) which report on structural and functional cardiovascular pathology, with an emphasis on imaging and disease pathophysiology. Articles must be authentic, educational, clinically relevant, and original in their content and scientific approach. IJC Heart & Vasculature requires the highest standards of scientific integrity in order to promote reliable, reproducible and verifiable research findings. All authors are advised to consult the Principles of Ethical Publishing in the International Journal of Cardiology before submitting a manuscript. Submission of a manuscript to this journal gives the publisher the right to publish that paper if it is accepted. Manuscripts may be edited to improve clarity and expression.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


