SGLT2抑制剂和GLP-1受体激动剂与2型糖尿病患者帕金森病风险的关联:一项倾向评分匹配的队列研究和荟萃分析
IF 7.4
3区 医学
Q1 ENDOCRINOLOGY & METABOLISM
引用次数: 0
摘要
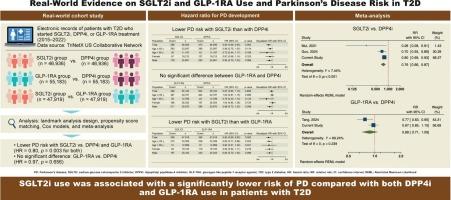
目的:本研究旨在探讨钠-葡萄糖共转运蛋白2抑制剂(SGLT2is)、胰高血糖素样肽-1受体激动剂(GLP-1RAs)与2型糖尿病(T2D)患者帕金森病(PD)风险之间的关系。方法:我们使用TriNetX美国研究网络进行了一项真实世界的队列研究。在2015年至2022年期间,年龄 ≥ 50 岁的T2D起始SGLT2is、GLP-1RAs或二肽基肽酶-4抑制剂(DPP4is)的成年人被纳入研究。采用新用户、主动比较器设计和倾向评分匹配进行里程碑式分析。主要结局是PD事件。还进行了一项纳入其他现实世界研究的荟萃分析。结果:SGLT2i与DPP4i、GLP-1RA与DPP4i、SGLT2i与GLP-1RA的比较共纳入93872例、110366例和95838例患者。SGLT2i用户的风险显著降低PD与DPP4i用户(HR = 0.80,95 % CI: 0.69 - -0.93, p = 0.003)和GLP-1RA用户(HR = 0.80,95 % CI: 0.69 - -0.93, p = 0.003)。GLP-1RA和DPP4i使用者之间无显著差异(HR = 0.97,95 % CI: 0.85-1.10, p = 0.656)。荟萃分析进一步支持SGLT2i使用与PD风险降低相关。结论:与使用DPP4i和GLP-1RA相比,使用SGLT2i与T2D患者发生PD的风险显著降低相关。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Association of SGLT2 inhibitors and GLP-1 receptor agonists with the risk of Parkinson’s disease in patients with type 2 diabetes: A propensity score–matched cohort study with meta-analysis
Aims
This study aimed to investigate the association between sodium-glucose cotransporter 2 inhibitors (SGLT2is), glucagon-like peptide-1 receptor agonists (GLP-1RAs), and the risk of Parkinson’s disease (PD) in patients with type 2 diabetes (T2D).
Methods
We conducted a real-world cohort study using the TriNetX U.S. Research Network. Adults aged ≥ 50 years with T2D initiating SGLT2is, GLP-1RAs, or dipeptidyl peptidase-4 inhibitors (DPP4is) between 2015 and 2022 were included. A landmark analysis using a new-user, active-comparator design with propensity score matching was applied. The primary outcome was incident PD. A meta-analysis incorporating additional real-world studies was also performed.
Results
In total, 93,872, 110,366, and 95,838 patients were included in the SGLT2i vs. DPP4i, GLP-1RA vs. DPP4i, and SGLT2i vs. GLP-1RA comparisons, respectively. SGLT2i users had a significantly lower risk of PD compared with both DPP4i users (HR = 0.80, 95 % CI: 0.69–0.93, p = 0.003) and GLP-1RA users (HR = 0.80, 95 % CI: 0.69–0.93, p = 0.003). No significant difference was observed between GLP-1RA and DPP4i users (HR = 0.97, 95 % CI: 0.85–1.10, p = 0.656). The meta-analysis further supported the reduced PD risk associated with SGLT2i use.
Conclusions
SGLT2i use was associated with a significantly lower risk of PD compared with both DPP4i and GLP-1RA use in patients with T2D.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Diabetes research and clinical practice
医学-内分泌学与代谢
CiteScore
10.30
自引率
3.90%
发文量
862
审稿时长
32 days
期刊介绍:
Diabetes Research and Clinical Practice is an international journal for health-care providers and clinically oriented researchers that publishes high-quality original research articles and expert reviews in diabetes and related areas. The role of the journal is to provide a venue for dissemination of knowledge and discussion of topics related to diabetes clinical research and patient care. Topics of focus include translational science, genetics, immunology, nutrition, psychosocial research, epidemiology, prevention, socio-economic research, complications, new treatments, technologies and therapy.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


