通过家用床垫下装置对美国男性和女性进行连续大样本的阻塞性睡眠呼吸暂停检测和患病率
IF 3.4
2区 医学
Q1 CLINICAL NEUROLOGY
引用次数: 0
摘要
背景:阻塞性睡眠呼吸暂停(OSA)经常未被诊断,阻碍了及时干预。这种情况与不良的心血管和代谢结果有关。目的调查美国大量真实世界样本中OSA的患病率,以及使用家庭床垫下睡眠监测设备检测OSA的夜间变异性。研究人员分析了2021年9月1日至2023年8月31日期间151013个个体年的睡眠追踪器-人工智能监测器记录的4700多万个夜晚的睡眠和呼吸数据。在两个为期一年的研究期间(9月至8月)中有至少300个夜晚记录的个体被纳入符合这一标准的第一年。对每个个体的每一年研究期进行分析,使用一年的平均AHI来确定OSA类别。研究人员分析了两个为期一年的队列中38,084名参与者(17,516名男性,15,360名女性和5208名未透露性别)的12,400,521个记录的夜晚。bmi正常(25kg/m2)人群中OSA (AHI≥5)患病率[95% CI]随年龄增加而增加:女性50岁,2.8% [2.2%,3.5%];女性≥50年,16.1% (14.6%,17.8%)(OR: 6.8 [5.2, 8.7]);男性50岁,11.2% [9.7%,12.7%];和男人≥50年,37.5% (34.8%,40.2%)(OR: 4.8[4.0, 5.7])。中度至重度和重度OSA受试者分别在5.1±7.6%和5.3±6.9%的夜间(平均±SD)显示出≥2级的严重程度降低(中度至正常或重度至轻度/正常)。随机选择3个夜晚的最大AHI值显示,1年内平均AHI值的敏感性/特异性[95% ci]分别为95.2%[94.2,96.1]/ 94.4%[94.2,94.7](中重度OSA)和95.6%[93.7,97.2]/ 98.0%[97.9,98.1](重度OSA)。结论osa患病率随年龄增长而增加,年龄≥50岁的男性和女性患病率均较高。同时,在中度至重度和重度OSA患者中,5.1%和5.3%的患者夜间的OSA分类比他们当年的平均AHI分类低2个类别。本文章由计算机程序翻译,如有差异,请以英文原文为准。
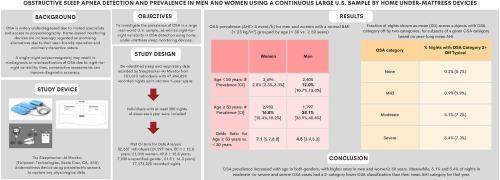
Obstructive sleep apnea detection and prevalence in men and women using a continuous large U.S. sample by home under-mattress devices
Background
Obstructive sleep apnea (OSA) often goes undiagnosed, hindering timely intervention. This condition is associated with adverse cardiovascular and metabolic outcomes.
Objectives
To investigate the prevalence of OSA in a large real-world U.S. sample, as well as night-to-night variability in OSA detection using home under-mattress sleep monitoring devices.
Methods
We analyzed de-identified sleep and respiratory data from over 47 million nights recorded by the Sleeptracker-AI Monitor in 151,013 individual-years between September 1, 2021, and August 31, 2023. Individuals with at least 300 recorded nights in one of two one-year study periods (September to August) were included on the first year they met this criterion. Each one-year study period for each individual was analyzed, with mean AHI for the one-year period used to determine OSA categories.
Results
A total of 12,400,521 recorded nights from 38,084 participants across the two one-year cohorts (17,516 men, 15,360 women, and 5208 undisclosed gender) were analyzed. OSA (AHI ≥5) prevalence [95 % CI] among individuals with normal BMIs (<25kg/m2) increased with age: women <50 years, 2.8 % [2.2 %, 3.5 %]; women ≥50 years, 16.1 % [14.6 %, 17.8 %] (OR: 6.8 [5.2, 8.7]); men <50 years, 11.2 % [9.7 %, 12.7 %]; and men ≥50 years, 37.5 % [34.8 %, 40.2 %] (OR: 4.8 [4.0, 5.7]). Moderate-to-severe and severe OSA subjects showed a ≥2-category severity reduction (moderate to normal or severe to mild/normal) on 5.1 ± 7.6 % and 5.3 ± 6.9 % of nights (mean ± SD), respectively. Maximum AHI values from 3 randomly selected nights demonstrated sensitivities/specificities [95 % CIs] of 95.2 % [94.2, 96.1]/94.4 % [94.2, 94.7] (moderate-to-severe OSA), and 95.6 % [93.7, 97.2]/98.0 % [97.9, 98.1] (severe OSA), categorized by mean AHI over 1 year.
Conclusion
OSA prevalence increased with age in both genders, with higher rates in men and women≥ 50 years. Meanwhile, 5.1 % and 5.3 % of nights in moderate-to-severe and severe OSA cases had a 2-category lower OSA classification than their mean AHI category for that year.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Sleep medicine
医学-临床神经学
CiteScore
8.40
自引率
6.20%
发文量
1060
审稿时长
49 days
期刊介绍:
Sleep Medicine aims to be a journal no one involved in clinical sleep medicine can do without.
A journal primarily focussing on the human aspects of sleep, integrating the various disciplines that are involved in sleep medicine: neurology, clinical neurophysiology, internal medicine (particularly pulmonology and cardiology), psychology, psychiatry, sleep technology, pediatrics, neurosurgery, otorhinolaryngology, and dentistry.
The journal publishes the following types of articles: Reviews (also intended as a way to bridge the gap between basic sleep research and clinical relevance); Original Research Articles; Full-length articles; Brief communications; Controversies; Case reports; Letters to the Editor; Journal search and commentaries; Book reviews; Meeting announcements; Listing of relevant organisations plus web sites.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


