间质性肺疾病的睡眠呼吸暂停:患病率、严重程度和危险因素的系统回顾和荟萃分析
IF 3.4
2区 医学
Q1 CLINICAL NEUROLOGY
引用次数: 0
摘要
背景:阻塞性睡眠呼吸暂停(OSA)在间质性肺疾病(ILD)患者中很常见,并影响疾病进展和预后。本荟萃分析旨在估计ILD患者的OSA患病率,并研究其与肺功能参数和危险因素的关系。方法检索spubmed、Embase和Cochrane图书馆,检索2025年2月前发表的评估ILD患者OSA患病率或呼吸暂停低通气指数(AHI)的研究。主要结局是OSA的患病率和严重程度(通过AHI评估)。次要结局评估用力肺活量(FVC)、肺一氧化碳弥散量(DLCO)、6分钟步行距离(6MWD)、BMI、吸烟率和男性百分比的影响。研究方案已在PROSPERO注册(CRD420250650698)。结果纳入17项研究,1092名受试者。荟萃分析显示,OSA患病率为68% (95% CI: 59 - 75%), IPF患者的患病率(71%,95% CI: 61 - 80%)高于非IPF患者。合并平均AHI为13.36 (95% CI: 10.87-16.41);中重度OSA患病率为36%。在多因素分析中,OSA患病率与低FVC (P = 0.086)、男性(P < 0.05)和BMI (P = 0.065 ~ 0.081)相关。AHI与6MWD (P = 0.086)和BMI (P = 0.065 ~ 0.084)轻度相关。亚组分析发现,FVC < 80% (P = 0.065)、6MWD < 372 m (P = 0.036)、BMI > 31 kg/m2 (P = 0.21)的ILD患者发生OSA的风险增加。结论:考虑到ILD患者中OSA的高患病率,建议进行常规筛查,尤其是FVC预测值为80%、BMI为31 kg/m2或6MWD为372 m的男性患者。早期发现可以及时干预并改善结果。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Sleep apnea in interstitial lung disease: A systematic review and meta-analysis of prevalence, severity, and risk factors
Background
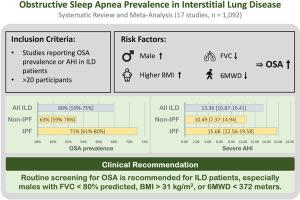
Obstructive sleep apnea (OSA) is common in interstitial lung disease (ILD) patients and affects disease progression and outcomes. This meta-analysis aims to estimate OSA prevalence in ILD and examine associations with lung function parameters and risk factors.
Methods
PubMed, Embase, and Cochrane Library were searched for studies assessing OSA prevalence or apnea-hypopnea index (AHI) in ILD, published before February 2025. Primary outcomes were OSA prevalence and severity (assessed by AHI). Secondary outcomes assessed the influence of forced vital capacity (FVC), diffusing capacity of the lungs for carbon monoxide (DLCO), 6-min walk distance (6MWD), BMI, smoking rate, and male percentage. The study protocol was registered in PROSPERO (CRD420250650698).
Results
17 studies comprising 1092 participants were included. Meta-analysis revealed an OSA prevalence of 68 % (95 % CI: 59–75 %), with higher rates in IPF (71 %, 95 % CI: 61–80 %) than non-IPF ILD. The pooled mean AHI was 13.36 (95 % CI: 10.87–16.41); moderate-to-severe OSA prevalence was 36 %. In multivariate analysis, OSA prevalence was associated with lower FVC (P = 0.086), male sex (P < 0.05), and BMI (P = 0.065–0.081). AHI was mildly associated with 6MWD (P = 0.086) and BMI (P = 0.065–0.084). Subgroup analyses identified that ILD patients with FVC < 80 % (P = 0.065), 6MWD < 372 m (P = 0.036), and BMI > 31 kg/m2 (P = 0.21) were at increased risk for OSA.
Conclusion
Given the high OSA prevalence in ILD patients, routine screening—particularly in males with FVC < 80 % predicted, BMI > 31 kg/m2, or 6MWD < 372 m—is recommended. Early detection may enable timely intervention and improve outcomes.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Sleep medicine
医学-临床神经学
CiteScore
8.40
自引率
6.20%
发文量
1060
审稿时长
49 days
期刊介绍:
Sleep Medicine aims to be a journal no one involved in clinical sleep medicine can do without.
A journal primarily focussing on the human aspects of sleep, integrating the various disciplines that are involved in sleep medicine: neurology, clinical neurophysiology, internal medicine (particularly pulmonology and cardiology), psychology, psychiatry, sleep technology, pediatrics, neurosurgery, otorhinolaryngology, and dentistry.
The journal publishes the following types of articles: Reviews (also intended as a way to bridge the gap between basic sleep research and clinical relevance); Original Research Articles; Full-length articles; Brief communications; Controversies; Case reports; Letters to the Editor; Journal search and commentaries; Book reviews; Meeting announcements; Listing of relevant organisations plus web sites.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


