主动脉瓣置换术治疗严重主动脉反流患者:比较二尖瓣和三尖瓣主动脉瓣的结果
IF 1.8
Q3 CARDIAC & CARDIOVASCULAR SYSTEMS
American heart journal plus : cardiology research and practice
Pub Date : 2025-09-12
DOI:10.1016/j.ahjo.2025.100617
引用次数: 0
摘要
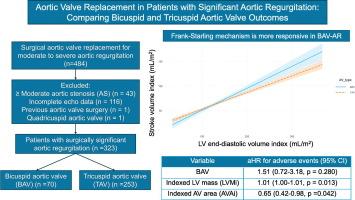
背景:在主动脉瓣置换术(SAVR)的主动脉瓣返流(AR)患者中,双尖瓣主动脉瓣(BAV)形态学在左室(LV)重构和预后中的作用尚不清楚。本研究比较了中重度AR患者的左室功能和术后结果,按BAV和三尖瓣主动脉瓣(TAV)形态分层。方法回顾性分析323例孤立性中重度AR行SAVR的患者(BAV: n = 70; TAV: n = 253)。评估基线临床、超声心动图、手术和随访资料。不良事件定义为全因死亡率和心力衰竭再住院的综合。结果BAV患者年龄小于10岁,症状较轻,但主动脉瓣指数面积(AVAi)较小,反流体积较大。BAV患者随着左室舒张末期指数容积(LVEDVi)的升高,其指数脑卒中容积(SVi)的升高幅度更大(p相互作用= 0.008);随着左室收缩末期直径(LVESD)的增大,其左室射血分数的下降幅度更轻(p相互作用= 0.004)。BAV患者的不良事件较少(16% vs 30%, p = 0.014)。AVAi和索引左室质量(LVMi)独立预测多变量调整和年龄匹配后的不良事件,而瓣膜形态不能预测。结论在孤立性AR需要SAVR的患者中,BAV患者在年轻时有更严重的瓣膜功能障碍,但更能保留左室扩张的收缩功能。AVAi和LVMi独立预测术后预后,支持其用于风险分层和及时干预,特别是在年轻的BAV患者中。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Aortic valve replacement in patients with significant aortic regurgitation: Comparing bicuspid and tricuspid aortic valve outcomes
Background
The role of bicuspid aortic valve (BAV) morphology in left ventricular (LV) remodelling and outcomes in aortic regurgitation (AR) patients undergoing surgical aortic valve replacement (SAVR) remains unclear. This study compares LV function and postoperative outcomes in patients with moderate-to-severe AR, stratified by BAV versus tricuspid aortic valve (TAV) morphology.
Methods
We retrospectively analyzed 323 patients with isolated moderate-to-severe AR undergoing SAVR (BAV: n = 70; TAV: n = 253). Baseline clinical, echocardiographic, surgical, and follow-up data were evaluated. Adverse events were defined as a composite of all-cause mortality and heart failure rehospitalization.
Results
Patients with BAV were a decade younger, were less symptomatic, but had smaller indexed aortic valve areas (AVAi) and greater regurgitant volumes. Patients with BAV had greater rise in indexed stroke volumes (SVi) with rising indexed LV end-diastolic volumes (LVEDVi) (pinteraction = 0.008), and milder LV ejection fraction decline with increasing LV end-systolic diameter (LVESD) (pinteraction = 0.004). Patients with BAV experienced less adverse events (16 % vs 30 %, p = 0.014). AVAi and indexed LV mass (LVMi) independently predicted adverse events after multivariable adjustment and age-matching, while valve morphology did not.
Conclusion
In patients requiring SAVR for isolated AR, patients with BAV had more severe valve dysfunction at a younger age but more preserved systolic function with LV dilation. AVAi and LVMi independently predict postoperative outcomes, supporting their use for risk stratification and timely intervention, especially in younger BAV patients.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

American heart journal plus : cardiology research and practice
Cardiology and Cardiovascular Medicine
CiteScore
1.60
自引率
0.00%
发文量
0
审稿时长
59 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


