气道超声评估对阻塞性睡眠呼吸暂停的评价——一项系统综述和荟萃分析。
IF 3.1
3区 医学
Q2 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
摘要
背景:超声(US)作为阻塞性睡眠呼吸暂停(OSA)的床边筛查工具受到关注,研究评估了各种参数。我们进行了这项系统综述和荟萃分析,以确定美国气道评估是否可以区分OSA和非OSA个体。方法:检索PubMed、Scopus、clinicaltrials.gov、GoogleScholar和Embase数据库,检索自成立之日至2024年7月1日期间报告使用多导睡眠图诊断OSA的颈部超声检查的研究。1703项研究被确定,在剔除重复研究后,筛选了798项研究。本系统综述评估了23项评估OSA筛查US参数的前瞻性、横断面和病例对照研究,并纳入了12项研究进行定量分析。计算OSA组和非OSA组之间各种US参数的加权平均差异。结果:在1008篇文献中,23篇被纳入系统评价,12篇进行了定量分析。12项研究中有11项采用纽卡斯尔-渥太华量表进行了高质量研究。研究中观察到显著的异质性,评估了OSA筛查的多个US参数。我们在meta分析中纳入了三个静态参数和两个动态参数;并计算出OSA与非OSA个体之间各维度的平均加权差(WMD)。舌动脉间距(WMD为4.43±3.05mm)、舌底平均厚度(WMD为6.34±4.86 mm)、咽侧壁厚度(WMD为3.59±1.99 mm)是区分OSA与非OSA个体的静态参数;动态参数包括吸气时腭后径(WMD -9.41±6.16 mm)、呼气时(WMD -6.10±2.61 mm)和muller’s手法(WMD -10.49±7.31 mm);吸气和呼气时舌后径分别为-3.84±1.46 mm和-2.27±1.39 mm。结论:舌动脉之间的距离增加,舌底平均厚度增加,咽侧壁增厚;或在吸气、呼气或穆勒氏手法时腭后直径减小;或吸气或呼气时舌后直径减小,始终能够区分OSA患者和非OSA患者。然而,标准化的临界值尚未得到,强调在推荐常规临床应用之前需要进行更大规模、方法学上统一的研究。本文章由计算机程序翻译,如有差异,请以英文原文为准。
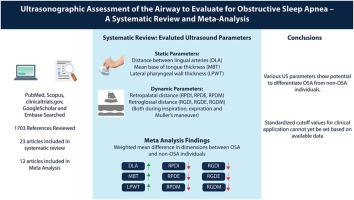
Ultrasonographic assessment of the airway to evaluate for obstructive sleep apnea – a systematic review and meta-analysis
Background
Ultrasound (US) has gained attention as a bedside screening tool for obstructive sleep apnea (OSA), with studies evaluating various parameters for its assessment. We conducted this systematic review and meta-analysis to determine whether US assessment of the airway can differentiate between OSA and Non-OSA individuals.
Methods
PubMed, Scopus, clinicaltrials.gov, GoogleScholar and Embase databases were searched from inception through July 01, 2024 for studies reporting neck ultrasonography in OSA, diagnosed using polysomnography. 1703 studies were identified, and after removing duplicate studies, 798 studies were screened. 23 prospective, cross sectional and case control studies evaluating US parameters for OSA screening were evaluated in the systematic review and 12 studies were included in the quantitative analysis. Weighted mean differences were calculated for various US parameters between OSA and non-OSA groups.
Results
Of the 1703 references reviewed, 23 articles were included in the systematic review and 12 underwent quantitative analysis. 11 of the 12 studies were found to be of high quality using Newcastle-Ottawa scale. Significant heterogeneity was observed across studies, with multiple US parameters assessed for OSA screening. We included three static and two dynamic parameters in the meta-analysis; and calculated mean weighted difference (WMD) in dimensions between OSA and non-OSA individuals. The static parameters that significantly differentiated OSA and non-OSA individuals were distance between lingual arteries (WMD 4.43 ± 3.05 mm), mean base of tongue thickness (WMD 6.34 ± 4.86 mm), and lateral pharyngeal wall thickness (WMD 3.59 ± 1.99 mm); while the dynamic parameters included retropalatal diameter during inspiration (WMD -9.41 ± 6.16 mm), expiration (WMD -6.10 ± 2.61 mm) and muller's maneuver (WMD -10.49 ± 7.31 mm); and retroglossal diameter during inspiration (WMD -3.84 ± 1.46 mm) and expiration (WMD -2.27 ± 1.39 mm).
Conclusions
Increased distance between the lingual arteries, greater mean tongue base thickness, and thicker lateral pharyngeal walls; or reduced retropalatal diameter during inspiration, expiration, or Muller's maneuver; or reduced retroglossal diameter during inspiration or expiration were consistently able to differentiate individuals with OSA from non-OSA individuals. However, standardized cutoff values are not yet available, underscoring the need for larger, methodologically uniform studies before routine clinical application can be recommended.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Respiratory medicine
医学-呼吸系统
CiteScore
7.50
自引率
0.00%
发文量
199
审稿时长
38 days
期刊介绍:
Respiratory Medicine is an internationally-renowned journal devoted to the rapid publication of clinically-relevant respiratory medicine research. It combines cutting-edge original research with state-of-the-art reviews dealing with all aspects of respiratory diseases and therapeutic interventions. Topics include adult and paediatric medicine, epidemiology, immunology and cell biology, physiology, occupational disorders, and the role of allergens and pollutants.
Respiratory Medicine is increasingly the journal of choice for publication of phased trial work, commenting on effectiveness, dosage and methods of action.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


