脑脊液分流术的表现、管理和结果的社会经济差异
IF 2.1
4区 医学
Q3 CLINICAL NEUROLOGY
引用次数: 0
摘要
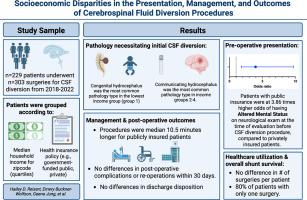
目的:探讨社会经济地位(SES)与社会弱势城市环境下学术中心脑脊液分流特征之间的关系。方法:我们回顾性分析229例患者(0.01-89岁)的303例手术,根据邮政编码的家庭收入中位数(即10万美元)和保险类型进行分组。结果:尽管医疗保险资格的年龄要求为65岁,但与私人保险患者相比,公共保险患者的手术年龄中位数明显年轻。需要脑脊液分流的病理在收入四分位数之间存在差异;沟通性脑积水在收入最高的人群中最常见,而先天性脑积水在收入最低的人群中最常见。结论:尽管先前报道了SES与手术结果之间的关联,但我们没有观察到两种SES指标在术后问题、出院处置或每位患者的手术次数方面存在统计学上的显著差异。医生应优先对患者进行颅内压升高症状的教育,并鼓励在出现这些症状时及时进行评估。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Socioeconomic Disparities in the Presentation, Management, and Outcomes of Cerebrospinal Fluid Diversion Procedures
Objective
We examined the relationship between socioeconomic status (SES) and features of cerebrospinal fluid (CSF) diversion at our academic center in a socially disadvantaged urban setting.
Methods
We retrospectively analyzed 303 surgeries among 229 patients (0.01–89 years), grouped according to median household income for zip-code (i.e., <$40,000, $40,000–$70,000, $70,000–$100,000, and >$100,000) and insurance type.
Results
The median age at surgery was significantly younger for publicly insured patients compared to privately insured patients, despite the 65-year age requirement for Medicare eligibility. Pathology necessitating CSF diversion differed across income quartiles; communicating hydrocephalus was most common in the highest group and congenital hydrocephalus was most common in the lowest income group (P < 0.05). Publicly insured patients were 3.86 times more likely to present with altered mental status than privately insured patients (95% confidence interval [CI]: 1.75–8.49; P < 0.001). Procedure duration and post-operative length-of-stay were longer for publicly than privately insured patients.
Conclusions
Despite previously reported associations between SES and surgical outcomes, we did not observe a statistically significant difference in post-operative issues, discharge disposition, or number of procedures per patient across two SES metrics. Physicians should prioritize educating patients about symptoms of elevated intracranial pressure and encourage prompt evaluation when these symptoms arise.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

World neurosurgery
CLINICAL NEUROLOGY-SURGERY
CiteScore
3.90
自引率
15.00%
发文量
1765
审稿时长
47 days
期刊介绍:
World Neurosurgery has an open access mirror journal World Neurosurgery: X, sharing the same aims and scope, editorial team, submission system and rigorous peer review.
The journal''s mission is to:
-To provide a first-class international forum and a 2-way conduit for dialogue that is relevant to neurosurgeons and providers who care for neurosurgery patients. The categories of the exchanged information include clinical and basic science, as well as global information that provide social, political, educational, economic, cultural or societal insights and knowledge that are of significance and relevance to worldwide neurosurgery patient care.
-To act as a primary intellectual catalyst for the stimulation of creativity, the creation of new knowledge, and the enhancement of quality neurosurgical care worldwide.
-To provide a forum for communication that enriches the lives of all neurosurgeons and their colleagues; and, in so doing, enriches the lives of their patients.
Topics to be addressed in World Neurosurgery include: EDUCATION, ECONOMICS, RESEARCH, POLITICS, HISTORY, CULTURE, CLINICAL SCIENCE, LABORATORY SCIENCE, TECHNOLOGY, OPERATIVE TECHNIQUES, CLINICAL IMAGES, VIDEOS
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


