非常规脂质参数预测心血管-肾-代谢综合征患者肾功能快速下降的风险:CHARLS的首个队列研究证据
IF 4.3
引用次数: 0
摘要
背景:本研究评估了三种新型脂质来源的生物标志物的预测价值:非hdl -to- hdl胆固醇比率(NHHR);残余胆固醇自然对数;胆固醇、高密度脂蛋白和葡萄糖指数(CHG)对心血管肾代谢(CKM)综合征患者快速肾功能下降(RKFD)的影响。方法:使用中国健康与退休纵向研究(CHARLS, 2011-2015)的数据,我们以RKFD为主要终点评估了2734例CKM患者(1-4期)。我们使用Logistic回归模型评估了NHHR、lnRC和CHG与肾脏预后的关系。使用限制三次样条和亚群分析来探索人口阶层之间的非线性关系和一致性。受试者工作特征(ROC)曲线分析比较了这些指标的预测性能。结果:经过完全调整的Logistic模型显示,NHHR单位增加与RKFD风险增加19. %相关(p )。结论:NHHR、lnRC和CHG与CKM患者的RKFD显著相关,是肾功能恶化的可靠预测因子。学习要点:本文章由计算机程序翻译,如有差异,请以英文原文为准。
Non-conventional lipid parameters predict the risk of rapid kidney function decline in patients with cardiovascular-kidney-metabolic syndrome: The first cohort study evidence from CHARLS
Background
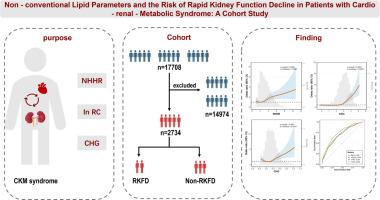
This study evaluates the predictive value of three novel lipid-derived biomarkers: non-HDL-to-HDL cholesterol ratio (NHHR); natural logarithm of remnant cholesterol (lnRC); and cholesterol, high-density lipoprotein, and glucose index (CHG) for rapid kidney function decline (RKFD) in patients with cardiovascular-kidney-metabolic (CKM) syndrome.
Methods
Using data from the China Health and Retirement Longitudinal Study (CHARLS, 2011–2015), we evaluated 2734 CKM patients (stages 1–4) using RKFD as the primary endpoint. We assessed the associations of NHHR, lnRC, and CHG with renal outcomes using Logistic regression models. Restricted cubic spline and subgroup analyses were used to explore nonlinear relationships and consistency across population strata. Receiver operating characteristic (ROC) curve analysis compared the predictive performance of these indices.
Results
Fully adjusted Logistic models showed that a unit increase in NHHR was associated with a 19 % increased RKFD risk (p < 0.001). LnRC and CHG demonstrated more pronounced effects, with risks increasing by 112 % and 125 % per unit, respectively (both p < 0.001). Restricted cubic splines analysis revealed a linear relationship for NHHR and “J-shaped” associations for lnRC and CHG. ROC analysis showed improved discriminative capacity, with receiver operating characteristic curve values of 0.694 (NHHR), 0.734 (lnRC), and 0.695 (CHG).
Conclusions
NHHR, lnRC, and CHG are significantly associated with RKFD in CKM patients and are robust predictors of renal function deterioration.
Key learning points
- •What was known: The existing rapid kidney function decline (RKFD) models for patients with cardiovascular-kidney-metabolic (CKM) syndrome lack sensitivity and often overlook the synergistic effect of glucose and lipid metabolism disorders on renal deterioration.
- •This study adds: The non-HDL-to-HDL cholesterol ratio; Natural Logarithm of Remnant Cholesterol (lnRC); and Cholesterol High-Density Lipoprotein, and Glucose index are strongly associated with RKFD, with lnRC demonstrating superior predictive accuracy over traditional risk factors, with identified thresholds for high-risk stratification.
- •Potential impact: Integrating these indices into standard clinical practice enhances the early detection of CKM syndrome patients at high risk of RKFD, thus permitting prompt intervention to deceler renal impairment and reduce the likelihood of progression to end-stage kidney disease.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Experimental gerontology
Ageing, Biochemistry, Geriatrics and Gerontology
CiteScore
6.70
自引率
0.00%
发文量
0
审稿时长
66 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


