尽管他汀类药物治疗,家族性高胆固醇血症患者的单核细胞仍具有炎症性
IF 2.1
Q3 PERIPHERAL VASCULAR DISEASE
引用次数: 0
摘要
背景和目的家族性高胆固醇血症(FH)以高胆固醇和早发心血管疾病为特征。虽然高胆固醇血症和炎症都是动脉粥样硬化斑块形成的关键驱动因素,但炎症在FH中的研究仍然不足。炎性(M1)巨噬细胞有助于斑块不稳定和巨噬细胞前体,单核细胞,可以偏向炎症状态。目的:确定;FH个体的单核细胞是否具有炎性,它们是否容易形成炎性巨噬细胞,以及在他汀类药物治疗的个体中是否仍然如此。方法采集FH患者(他汀治疗组和未治疗组)和健康对照者的血液样本。通过全血流式细胞术检测脂质谱和单核细胞炎症标志物的表达。用自体血清培养单核细胞,用流式细胞术测定巨噬细胞谱。结果fh治疗组总胆固醇和低密度脂蛋白胆固醇(LDL-C)高于fh治疗组和对照组。fh治疗组和未治疗组单核细胞均呈炎性,CD86 (M1)升高。在整个队列中,炎症/抗炎标志物(CD86/CD163)的比值与LDL-C和ApoB/ApoA1比值显著相关,表明FH的高LDL-C可能促进炎症单核细胞谱。来自(治疗)FH个体的单核细胞衍生巨噬细胞也具有更多的炎症谱(CD86和CD86/CD163)。总体而言,FH个体的单核细胞表现出炎症偏态,即使是胆固醇水平适度降低的个体。这些单核细胞很容易变成炎性巨噬细胞。这与随后的炎性巨噬细胞形成一起,可能导致斑块不稳定和下游临床事件。这支持炎症单核细胞靶向作为减少FH个体残留风险的潜在方法。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Monocytes from people with Familial Hypercholesterolaemia are inflammatory, despite statin-treatment
Background and aims
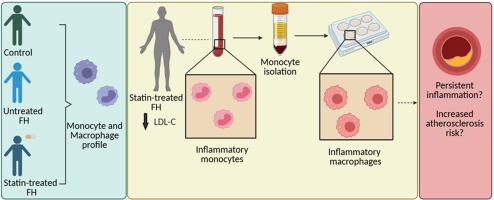
Familial Hypercholesterolaemia (FH) is characterised by high cholesterol and premature cardiovascular disease. While hypercholesterolaemia and inflammation are both key drivers in the formation of atherosclerotic plaques, inflammation remains understudied in FH. Inflammatory (M1) macrophages contribute to plaque destabilisation and macrophage precursors, monocytes, can be skewed towards an inflammatory state. Aims: Determine; whether monocytes of FH individuals are inflammatory, if they readily form inflammatory macrophages, and whether this remains so in statin-treated individuals.
Methods
Blood samples were collected from people with FH (statin-treated and untreated) and healthy controls. Lipid profile was obtained and monocyte inflammatory marker expression was determined by whole blood flow cytometry. Monocytes were cultured with autologous serum and resultant macrophage profile determined by flow cytometry.
Results
Total cholesterol and low-density lipoprotein cholesterol (LDL-C) were higher in the Untreated-FH group compared to the Treated-FH group and controls. In both Treated-FH and Untreated-FH groups, monocytes were inflammatory with high CD86 (M1). The ratio of inflammatory/anti-inflammatory markers (CD86/CD163) significantly correlated with LDL-C and ApoB/ApoA1 ratio across the cohort, indicating the high LDL-C of FH may promote an inflammatory monocyte profile. Monocyte-derived-macrophages from (Treated) FH individuals also had a more inflammatory profile (CD86 and CD86/CD163).
Conclusions
Overall, monocytes show inflammatory skewing in FH individuals, even those with moderately-reduced cholesterol levels. These monocytes readily become inflammatory macrophages. This, along with subsequent inflammatory macrophage formation, could contribute to plaque destabilisation and downstream clinical events. This supports inflammatory monocyte targeting as a potential approach to reduce residual risk in FH individuals.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Atherosclerosis plus
Cardiology and Cardiovascular Medicine
CiteScore
2.60
自引率
0.00%
发文量
0
审稿时长
66 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


