静态和动态瞳孔变化反映了健康成人急性睡眠剥夺的自主神经效应
IF 3.4
2区 医学
Q1 CLINICAL NEUROLOGY
引用次数: 0
摘要
目的通过比较急性睡眠剥夺受试者(≤4小时)和非睡眠剥夺对照组(≤7小时)的瞳孔活动和交感皮肤反应,评估急性睡眠剥夺受试者(≤4小时)的瞳孔活动和交感皮肤反应。方法39例受试者,其中睡眠剥夺组23例,健康对照组16例。采用自我报告睡眠时间、卡罗林斯卡嗜睡量表(KSS)和Epworth嗜睡量表(ESS)评估困倦状态。使用Sirius地形测量仪进行静态和动态瞳孔测量,使用Tonoref III进行调节幅度测量,并通过肌电图量化交感皮肤反应。结果急性睡眠剥夺组的平均暗瞳直径和中瞳直径均高于对照组(暗瞳亮度为6.33±0.59 vs 6.05±0.51,P = 0.030;中瞳亮度为5.28±0.69 vs 5.00±0.46,P = 0.047)。在动态瞳孔测量中,睡眠剥夺组瞳孔扩张速度明显高于对照组(0.22±0.03 vs 0.20±0.03,P = 0.004)。两组的光瞳直径、调节幅度和交感皮肤反应相似(P > 0.05)。在所有亮度下,睡眠时间与瞳孔直径呈负相关,而ESS评分与中视、光视瞳孔直径呈正相关(P < 0.05)。结论急性睡眠剥夺会改变静态和动态瞳孔反应,反映自主神经的变化,而皮肤交感神经反应不受影响。即使是一天的部分睡眠剥夺也会损害瞳孔的反应。本文章由计算机程序翻译,如有差异,请以英文原文为准。
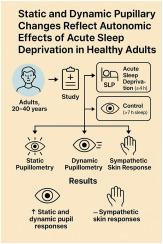
Static and dynamic pupillary changes reflect autonomic effects of acute sleep deprivation in healthy adults
Aim
To assess the pupillary activity and sympathetic skin responses of acute sleep-deprived participants (≤4 h) by comparing these values with non-sleep-deprived controls (>7 h).
Methods
This study included 39 participants, comprising 23 from the sleep deprivation group and 16 from the healthy control group. Self-reported sleep duration, the Karolinska Sleepiness Scale (KSS), and the Epworth Sleepiness Scale (ESS) were used to evaluate the state of sleepiness. Static and dynamic pupillometry measurements using the Sirius topography device, the amplitude of accommodation using Tonoref III, and sympathetic skin responses quantified via EMG were examined.
Results
The mean scotopic and mesopic pupil diameters were higher in acute sleep-deprived participants compared to controls (6.33 ± 0.59 vs 6.05 ± 0.51, P = 0.030 for scotopic luminance; 5.28 ± 0.69 vs 5.00 ± 0.46, P = 0.047 for mesopic luminance, respectively). In dynamic pupillometry, the speed of pupil dilation in the sleep deprivation group was higher than in the control group (0.22 ± 0.03 vs 0.20 ± 0.03, P = 0.004). The photopic pupil diameter, accommodation amplitude, and sympathetic skin responses were similar between the groups (P > 0.05). While sleep duration was inversely correlated with pupil diameters under all luminances, the ESS score was positively correlated with mesopic and photopic pupil diameters (P < 0.05 for each).
Conclusions
Acute sleep deprivation alters both static and dynamic pupil responses, reflecting autonomic changes, whereas sympathetic skin responses remained unaffected. Even a single day of partial sleep deprivation is capable of impairing pupillary responses.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Sleep medicine
医学-临床神经学
CiteScore
8.40
自引率
6.20%
发文量
1060
审稿时长
49 days
期刊介绍:
Sleep Medicine aims to be a journal no one involved in clinical sleep medicine can do without.
A journal primarily focussing on the human aspects of sleep, integrating the various disciplines that are involved in sleep medicine: neurology, clinical neurophysiology, internal medicine (particularly pulmonology and cardiology), psychology, psychiatry, sleep technology, pediatrics, neurosurgery, otorhinolaryngology, and dentistry.
The journal publishes the following types of articles: Reviews (also intended as a way to bridge the gap between basic sleep research and clinical relevance); Original Research Articles; Full-length articles; Brief communications; Controversies; Case reports; Letters to the Editor; Journal search and commentaries; Book reviews; Meeting announcements; Listing of relevant organisations plus web sites.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


