睡眠状态对血脂和2型糖尿病发病率的影响:中国人群队列的中介分析
IF 7.4
3区 医学
Q1 ENDOCRINOLOGY & METABOLISM
引用次数: 0
摘要
目的:本研究旨在探讨睡眠状态与2型糖尿病发病率之间的关系,并探讨脂质谱的潜在介导作用。方法:一项针对69116名年龄在20-74岁之间的上海参与者(2016-2019)的队列研究,追踪新发T2DM病例至2024年。使用匹兹堡睡眠质量指数(PSQI)评估睡眠状态。Cox和logistic回归模型评估了睡眠、血脂和T2DM之间的关系。通过中介分析探讨脂质谱的影响,包括甘油三酯(TG)、总胆固醇(TC)、高密度脂蛋白胆固醇(HDL-C)、低密度脂蛋白胆固醇(LDL-C)、血脂异常和中国内脏脂肪指数(CVAI)。结果:在49,734名符合条件的参与者中,有4,126例新诊断的T2DM病例。整体睡眠质量差(HR: 1.087, 95 % CI: 1.016, 1.162)、主观睡眠质量(HR: 1.097, 95 % CI: 1.007, 1.194)和睡眠障碍(HR: 1.118, 95 % CI: 1.038, 1.204)与T2DM的高风险相关。中介分析显示,血脂异常、TC和CVAI在睡眠障碍与2型糖尿病的关联中起主要中介作用。结论:睡眠障碍与较高的2型糖尿病风险有关,脂质谱介导了这一关系。控制脂质代谢和评估睡眠障碍患者的2型糖尿病风险是预防的关键。本文章由计算机程序翻译,如有差异,请以英文原文为准。
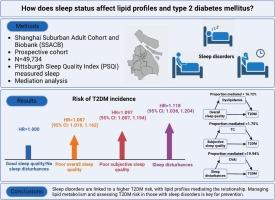
The impact of sleep status on lipid profiles and incident type 2 diabetes mellitus: a mediation analysis in a Chinese population cohort
Aims
This study aimed to examine the association between sleep status and T2DM incidence, and explore the potential mediating role of lipid profiles.
Methods
A cohort study of 69,116 participants aged 20–74 in Shanghai (2016–2019) tracked new T2DM cases until 2024. Sleep status was assessed using the Pittsburgh Sleep Quality Index (PSQI). Cox and logistic regression models evaluated the associations between sleep, lipid profiles, and T2DM. Mediation analysis was conducted to explore the effects of lipid profiles, including triglycerides (TG), total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), dyslipidemia, and the Chinese Visceral Adiposity Index (CVAI).
Results
Among 49,734 eligible participants, 4,126 new T2DM cases were diagnosed. Poor overall sleep quality (HR: 1.087, 95 % CI: 1.016, 1.162), subjective sleep quality (HR: 1.097, 95 % CI: 1.007, 1.194), and sleep disturbances (HR: 1.118, 95 % CI: 1.038, 1.204) were associated with a higher risk of T2DM. Mediation analysis revealed that dyslipidemia, TC, and CVAI played a major mediating role in the association between sleep disorders and T2DM.
Conclusions
Sleep disorders are linked to a higher T2DM risk, with lipid profiles mediating the relationship. Managing lipid metabolism and assessing T2DM risk in those with sleep disorders is key for prevention.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Diabetes research and clinical practice
医学-内分泌学与代谢
CiteScore
10.30
自引率
3.90%
发文量
862
审稿时长
32 days
期刊介绍:
Diabetes Research and Clinical Practice is an international journal for health-care providers and clinically oriented researchers that publishes high-quality original research articles and expert reviews in diabetes and related areas. The role of the journal is to provide a venue for dissemination of knowledge and discussion of topics related to diabetes clinical research and patient care. Topics of focus include translational science, genetics, immunology, nutrition, psychosocial research, epidemiology, prevention, socio-economic research, complications, new treatments, technologies and therapy.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


