极低胎龄新生儿急性肾损伤及继发迟发性感染风险
IF 2.4
3区 医学
Q2 OBSTETRICS & GYNECOLOGY
引用次数: 0
摘要
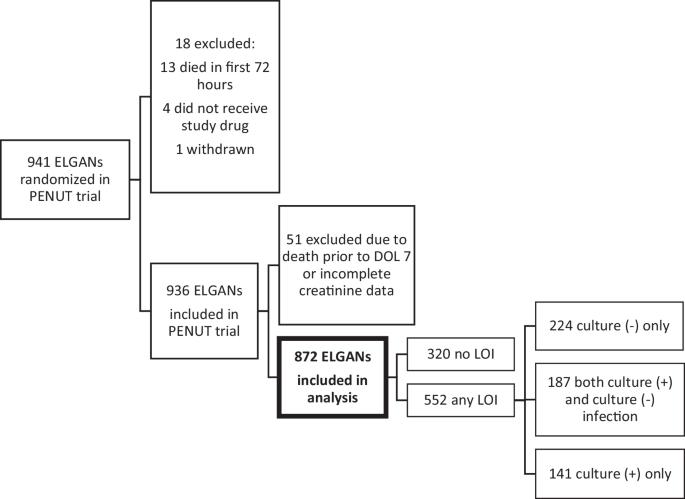
目的:确定极低胎龄新生儿(ELGAN)急性肾损伤(AKI)是否与随后的迟发性感染(LOI)相关。研究设计:对早产儿促红细胞生成素神经保护试验参与者进行二次分析。存活≥7天且血清肌酐数据充足的婴儿纳入研究。主要终点为AKI后≥72小时开始的LOI。时变Cox比例风险模型估计AKI和LOI的调整风险比。结果:332/872(38%)的研究婴儿经历AKI。552/872(63%)经历过LOI。迟发性感染336/552例(60.9%)培养阳性,216/552例(39.1%)培养阴性。在调整胎龄、性别、产后类固醇、万古霉素/庆大霉素接受≥72小时、出生体重和5分钟APGAR后,任何AKI与随后LOI的风险增加1.47倍相关(调整HR: 1.47; 95% CI: 1.15-1.87)。结论:在大量elgan患者中,既往AKI增加了随后LOI的风险。临床医生可能预期AKI后感染并发症的风险更高。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Acute kidney injury and subsequent risk of late-onset infection among extremely low gestational age newborns
Determine whether acute kidney injury (AKI) is associated with subsequent late-onset infection (LOI) among extremely low gestational age newborns (ELGAN). Secondary analysis of participants in the Preterm Erythropoietin for Neuroprotection Trial. Infants surviving ≥7 days with sufficient serum creatinine data were included. The primary outcome was any LOI, starting ≥72 h after AKI. Time-varying Cox proportional hazards modeling estimated adjusted hazard ratios of AKI and LOI. 332/872 (38%) study infants experienced AKI. 552/872 (63%) experienced LOI. 336/552 (60.9%) of late-onset infections were culture-positive, and 216/552 (39.1%) were culture-negative. After adjusting for gestational age, sex, postnatal steroids, vancomycin/gentamicin receipt ≥72 h, birthweight, and 5-min APGAR, any AKI was associated with 1.47x increased hazard of subsequent LOI (adjusted HR: 1.47; 95% CI: 1.15–1.87). Prior AKI increased hazard of subsequent LOI in a large cohort of ELGANs. Clinicians may anticipate higher risk of infectious complications after AKI.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Journal of Perinatology
医学-妇产科学
CiteScore
5.40
自引率
6.90%
发文量
284
审稿时长
3-8 weeks
期刊介绍:
The Journal of Perinatology provides members of the perinatal/neonatal healthcare team with original information pertinent to improving maternal/fetal and neonatal care. We publish peer-reviewed clinical research articles, state-of-the art reviews, comments, quality improvement reports, and letters to the editor. Articles published in the Journal of Perinatology embrace the full scope of the specialty, including clinical, professional, political, administrative and educational aspects. The Journal also explores legal and ethical issues, neonatal technology and product development.
The Journal’s audience includes all those that participate in perinatal/neonatal care, including, but not limited to neonatologists, perinatologists, perinatal epidemiologists, pediatricians and pediatric subspecialists, surgeons, neonatal and perinatal nurses, respiratory therapists, pharmacists, social workers, dieticians, speech and hearing experts, other allied health professionals, as well as subspecialists who participate in patient care including radiologists, laboratory medicine and pathologists.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


