降脂药物对脂蛋白升高个体氧化磷脂的影响(a)
IF 2.1
Q3 PERIPHERAL VASCULAR DISEASE
引用次数: 0
摘要
氧化磷脂(OxPLs)与载脂蛋白B-100 (OxPL-apoB)和载脂蛋白(a) [OxPL-apo(a)]结合,并自由存在于含载脂蛋白的磷脂壳内。OxPLs与脂蛋白的促炎特性有关(a) [Lp(a)]。携带纤溶酶原(OxPL-PLG)的oxpl可延长纤溶时间。目的探讨降脂药物对Lp(a)浓度升高患者OxPLs水平的影响。方法在本前瞻性研究中,Lp(a)水平≥75 nmol/L的患者(n = 70)根据现行指南分为3个治疗方案:高强度他汀单药治疗(n = 28),在高强度他汀基础上加依泽替米贝(n = 31),在高强度他汀+依泽替米贝基础上加蛋白转化酶subtilisin/ keexin 9型抑制剂(PCSK9i)治疗(n = 11)。随访时间3个月。结果患者平均年龄为51±15岁,40%为男性,39%诊断为家族性高胆固醇血症,16%患有动脉粥样硬化性心血管疾病,36%、33%和15%分别为心血管高危、高危和中度风险。Lp(a)水平在高强度他汀类药物和加用依折替布治疗组无显著变化,但在加用PCSK9i治疗组显著降低。高强度他汀类药物和附加依可替米贝组OxPL-apoB和OxPL-apo(a)均显著升高,OxPL-PLG均显著降低。附加PCSK9i治疗与OxPL-apoB、OxPL-apo(a)和OxPL-PLG水平无显著变化相关。结论在Lp(a)升高的患者中,高强度他汀和加药依泽替米贝均可显著提高OxPL-apoB和OxPL-apo(a)水平,同时显著降低OxPL-PLG水平。添加PCSK9i对OxPLs水平无显著影响。这些发现的临床意义有待进一步探讨。本文章由计算机程序翻译,如有差异,请以英文原文为准。
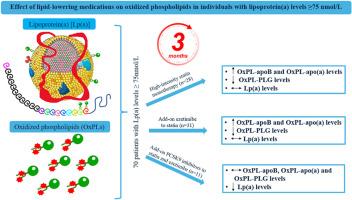
Effect of lipid-lowering medications on oxidized phospholipids in individuals with elevated LIPOPROTEIN(a)
Background/introduction
Oxidized phospholipids (OxPLs) are bound to apolipoprotein B-100 (OxPL-apoB) and apolipoprotein(a) [OxPL-apo(a)] and are present freely within the phospholipid shell of apoB-containing lipoproteins. OxPLs have been linked with the pro-inflammatory properties of lipoprotein(a) [Lp(a)]. OxPLs carried on plasminogen (OxPL-PLG) may extend the time to fibrinolysis.
Purpose
To evaluate the effect of lipid-lowering medications on OxPLs levels in individuals with elevated Lp(a) concentrations.
Methods
In this prospective study, patients (n = 70) with Lp(a) levels ≥75 nmol/L were assigned to 3 treatment regimens according to current guidelines: high-intensity statin monotherapy (n = 28), ezetimibe added to high-intensity statin (n = 31) and proprotein convertase subtilisin/kexin type 9 inhibitor (PCSK9i) added to high-intensity statin plus ezetimibe (n = 11). Follow-up duration was 3 months.
Results
Patients had a mean age of 51 ± 15 years, 40 % were male, 39 % were diagnosed with familial hypercholesterolemia, 16 % had atherosclerotic cardiovascular disease, and 36 %, 33 % and 15 % were at very high, high, and moderate cardiovascular risk, respectively. Lp(a) levels did not change significantly with high-intensity statin and add-on ezetimibe but significantly decreased with add-on PCSK9i treatment. OxPL-apoB and OxPL-apo(a) significantly increased, while OxPL-PLG significantly decreased with both high-intensity statin and add-on ezetimibe. Add-on PCSK9i treatment was associated with no significant changes in OxPL-apoB, OxPL-apo(a) and OxPL-PLG levels.
Conclusions
Among patients with elevated Lp(a), both high-intensity statin and add-on ezetimibe significantly increased OxPL-apoB and OxPL-apo(a) levels, while significantly decreased OxPL-PLG levels. Add-on PCSK9i had no significant effect on OxPLs levels. The clinical implications of these findings should be further explored.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Atherosclerosis plus
Cardiology and Cardiovascular Medicine
CiteScore
2.60
自引率
0.00%
发文量
0
审稿时长
66 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


