重新利用他汀类药物治疗预防胆结石疾病
IF 5.7
2区 医学
Q1 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
摘要
背景和目的在观察性研究中,他汀类药物治疗与胆结石疾病(GSD)或胆囊切除术的低风险相关。我们测试了HMGCR的遗传变异,模拟他汀类药物治疗,在普通人群中降低GSD和胆囊切除术的风险的假设。方法使用来自哥本哈根普通人群研究(CGPS)和英国生物银行(UKBB)的101,809和375,094名个体的个体参与者数据进行药物靶向孟德尔随机化分析,中位随访时间分别为44年和26年,并使用多达1,319,534名个体的汇总数据进行外部验证。暴露的是HMGCR rs12654264A>;T,这是一种与低密度脂蛋白胆固醇(LDL- c)密切相关的GWAS变体。终点为GSD事件和胆囊切除术,阳性对照为心肌梗死(MI)。结果通过工具变量分析,他汀类药物治疗导致的LDL-C降低1个标准差(SD)与GSD风险降低21%和16%观察相关[优势比(OR) = 0.79(95% CI: 0.66-0.95)];CGPS和UKBB分别为0.84(0.78-0.91)。CGPS组和UKBB组相应的胆囊切除术风险分别降低12%[0.88(0.69-1.11)]和23%[0.77(0.71-0.84)]。在荟萃分析中,GSD患者通过HMGCR降低LDL-C每1 SD的OR为0.63(0.46-0.86),胆囊切除术患者为0.68(0.52-0.88),与MI患者的OR为0.75(0.63 - 0.88)相似。结论在普通人群中,他汀类药物治疗可能降低GSD和胆囊切除术的风险。此外,通过他汀类药物治疗降低LDL-C在预防GSD和胆囊切除术方面可能与预防心肌梗死一样有效。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Repurposing statin treatment for the prevention of gallstone disease
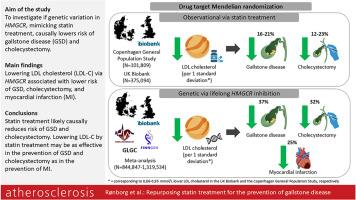
Background and aims
In observational studies, statin treatment has been associated with low risk of gallstone disease (GSD) or cholecystectomy. We tested the hypothesis that genetic variation in HMGCR, mimicking statin treatment, causally lowers risk of GSD and cholecystectomy in the general population.
Methods
A drug-target Mendelian randomization analysis was conducted using individual participant data on 101,809 and 375,094 individuals from the Copenhagen General Population Study (CGPS) and the UK Biobank (UKBB), followed for a median 44 and 26 years, respectively, with external validation using summary level data from up to 1,319,534 individuals. The exposure was HMGCR rs12654264A>T, a GWAS variant strongly associated with LDL cholesterol (LDL-C) in the Global Lipids Genetics Consortium. Endpoints were incident GSD and cholecystectomy, with myocardial infarction (MI) as a positive control.
Results
Using instrumental variable analysis, a 1 standard deviation (SD) lower LDL-C due to statin treatment was observationally associated with a 21 % and 16 % lower risk of GSD [Odds Ratio (OR) = 0.79(95 % CI:0.66–0.95)]; 0.84(0.78–0.91)] in the CGPS and UKBB, respectively. The corresponding risk of cholecystectomy was lower by 12 % [0.88(0.69–1.11)] and 23 % [0.77(0.71–0.84)] in the CGPS and UKBB, respectively. In meta-analyses, the ORs per 1 SD lower LDL-C via HMGCR were 0.63(0.46–0.86) for GSD and 0.68(0.52–0.88) for cholecystectomy, similar to the OR for MI of 0.75(0.63–0.88).
Conclusions
Statin treatment likely causally reduces risk of GSD and cholecystectomy in the general population. Furthermore, lowering LDL-C by statin treatment may be as effective in the prevention of GSD and cholecystectomy as in the prevention of MI.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Atherosclerosis
医学-外周血管病
CiteScore
9.80
自引率
3.80%
发文量
1269
审稿时长
36 days
期刊介绍:
Atherosclerosis has an open access mirror journal Atherosclerosis: X, sharing the same aims and scope, editorial team, submission system and rigorous peer review.
Atherosclerosis brings together, from all sources, papers concerned with investigation on atherosclerosis, its risk factors and clinical manifestations. Atherosclerosis covers basic and translational, clinical and population research approaches to arterial and vascular biology and disease, as well as their risk factors including: disturbances of lipid and lipoprotein metabolism, diabetes and hypertension, thrombosis, and inflammation. The Editors are interested in original or review papers dealing with the pathogenesis, environmental, genetic and epigenetic basis, diagnosis or treatment of atherosclerosis and related diseases as well as their risk factors.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


