神经发育障碍儿童的睡眠障碍:ASD、ADHD和对照组的比较活动描记和问卷评估
IF 3.4
2区 医学
Q1 CLINICAL NEUROLOGY
引用次数: 0
摘要
睡眠障碍在患有神经发育障碍(NDD)的儿童中非常普遍,但很少有研究将客观和主观的测量结合起来。本研究的目的是评估ADHD儿童和ASD儿童的睡眠模式和睡眠卫生,比较年龄匹配的正常发育儿童,使用父母报告的问卷调查和活动记录仪,评估这些测量之间的一致性,并确定活动记录仪在这一人群中的临床适用性。方法60例NDD患儿(30例ASD, 30例ADHD)和40例正常发育对照,年龄匹配,进行7夜的活动记录仪记录。家长完成儿童睡眠障碍量表(SDSC)和家庭睡眠习惯量表(FISH)。结果NDD组患者对活动描记术的耐受性良好(88%),与之前的研究结果一致。与TD对照组相比,ndd患儿的SDSC评分显著较高(p < 0.001),活动睡眠参数较差,包括睡眠效率较低(82.0% vs 87.3%, p < 0.001),睡眠后醒来时间较长(78.8 vs 52.7 min, p < 0.001)。活动记录仪与SDSC的一致性有限(NDD约53%,TD约15%)。在睡眠卫生方面没有发现显著的组间差异,尽管FISH评分仅在对照组中与选定的活动图参数相关。结论睡眠障碍在NDD中非常普遍,活动描记术是一种可靠且耐受性良好的临床评估工具。鉴于活动记录法和问卷调查之间的有限一致性,可能需要多种方法的方法。应考虑将活动记录仪纳入常规临床实践,以改善儿童NDD人群的睡眠评估。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Sleep disorders in children with neurodevelopmental disorders: Comparative actigraphy and questionnaire assessment in ASD, ADHD, and controls
Background
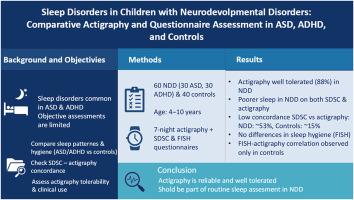
Sleep disturbances are highly prevalent in children with neurodevelopmental disorders (NDD), yet few studies have combined objective and subjective measures. The objectives of this study were to evaluate sleep patterns and sleep hygiene in children with ADHD and ASD compared age-matched typically developing children, using both parent-reported questionnaires and actigraphy, to assess the concordance between these measures, and to determine the clinical applicability of actigraphy in this population.
Methods
Sixty children with NDD (30 ASD, 30 ADHD) and 40 typically developing controls, matched for age, underwent seven nights of actigraphic recording. Parents completed the Sleep Disturbance Scale for Children (SDSC) and Family Inventory of Sleep Habits (FISH).
Results
Actigraphy was well tolerated in the NDD group (88 %), consistent with previous findings. Compared to TD controls, children with NDDs showed significantly higher SDSC scores (p < 0.001) and poorer actigraphic sleep parameters, including lower sleep efficiency (82.0 % vs 87.3 %, p < 0.001) and longer wake after sleep onset (78.8 vs 52.7 min, p < 0.001). Concordance between actigraphy and SDSC was limited (≈53 % in NDD; 15 % in TD). No significant group differences were found in sleep hygiene, although FISH scores correlated with selected actigraphic parameters only in controls.
Conclusions
Sleep disturbances are highly prevalent in NDD, and actigraphy is a reliable, well-tolerated tool for clinical assessment. Given the limited agreement between actigraphy and questionnaires, multimethod approaches may be necessary. Actigraphy should be considered for integration into routine clinical practice to improve sleep evaluation in pediatric NDD populations.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Sleep medicine
医学-临床神经学
CiteScore
8.40
自引率
6.20%
发文量
1060
审稿时长
49 days
期刊介绍:
Sleep Medicine aims to be a journal no one involved in clinical sleep medicine can do without.
A journal primarily focussing on the human aspects of sleep, integrating the various disciplines that are involved in sleep medicine: neurology, clinical neurophysiology, internal medicine (particularly pulmonology and cardiology), psychology, psychiatry, sleep technology, pediatrics, neurosurgery, otorhinolaryngology, and dentistry.
The journal publishes the following types of articles: Reviews (also intended as a way to bridge the gap between basic sleep research and clinical relevance); Original Research Articles; Full-length articles; Brief communications; Controversies; Case reports; Letters to the Editor; Journal search and commentaries; Book reviews; Meeting announcements; Listing of relevant organisations plus web sites.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


