基于纳米孔测序的宏基因组学新一代测序在临床感染病例中的预后价值:一项回顾性观察研究
IF 1.8
4区 医学
Q3 INFECTIOUS DISEASES
Diagnostic microbiology and infectious disease
Pub Date : 2025-09-02
DOI:10.1016/j.diagmicrobio.2025.117092
引用次数: 0
摘要
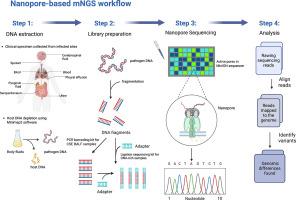
目的评价纳米孔测序技术(NST)与传统培养方法在感染性疾病病例中对新一代宏基因组测序(mNGS)的预后价值。方法采用回顾性、单中心观察性研究,比较NST组患者和标本类型与培养对照组的临床结果。采用Cox比例风险回归和Kaplan-Meier生存分析来评估诊断策略与28天死亡率之间的关系。为了减少偏差,采用倾向评分匹配(PSM)和稳健的多变量Cox回归分析来控制混杂因素。通过计算敏感性、特异性、阳性预测值(PPV)和阴性预测值(NPV)来量化诊断准确性。结果多变量Cox回归分析显示,基于nst的诊断与显著降低的28天死亡率独立相关。(HR = 0.29, 95% CI:0.09-0.91, p = 0.033)。NST检测细菌的敏感性为0.93,特异性为0.54,阳性预测值(PPV)为0.5,阴性预测值(NPV)为0.94。此外,NST组与较高的抗生素降级率(ADE)和缩短的治疗持续时间(DOT)相关,p值分别为0.0238和0.008。结论基于nst的mNGS在诊断细菌感染方面优于传统培养方法。NST组和阳性病原体检测与28天死亡率降低相关。此外,入院时较高的APACHE II评分被确定为预后较差的独立预测因子,强调了早期严重程度评估对患者预后的重要性。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Prognostic value of Nanopore sequencing-based metagenomics next-generation sequencing in clinical infectious cases: A retrospective observational study
Objectives
This study aimed to evaluate the prognostic value of metagenomic next-generation sequencing(mNGS) using Nanopore sequencing technology (NST) versus traditional culture methods in infectious disease cases.
Methods
We conducted a retrospective, single-center observational study comparing clinical outcomes between patients and specimen types in NST group and those in culture-based control group. Cox Proportional Hazards regression and Kaplan-Meier survival analysis were conducted to evaluate the association between diagnostic strategy and 28-day mortality. To minimize bias, Propensity Score Matching (PSM) and robust multivariate Cox regression analysis were employed to control for confounding factors. Diagnostic accuracy was quantified by calculating sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV).
Results
The NST-based diagnosis was independently associated with a significantly reduced 28-day mortality rate, as indicated by the robust multivariate Cox regression analysis. (HR = 0.29, 95 %CI:0.09-0.91, p = 0.033). The sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of NST in detecting bacterium were 0.93,0.54, 0.5and 0.94, respectively. Additionally, the NST group was associated with higher Antibiotic De-escalation Rate (ADE) and reduced Duration of Therapy (DOT), with p values of 0.0238 and 0.008, respectively.
Conclusion
NST-based mNGS demonstrated superior performance in diagnosing bacterial infections compared to traditional culture methods. The NST group and positive pathogen detection were associated with a reduced 28-day mortality rate. Additionally, higher APACHE II scores upon admission were identified as independent predictors of worse prognosis, highlighting the importance of early severity assessment in patient outcomes.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
CiteScore
5.30
自引率
3.40%
发文量
149
审稿时长
56 days
期刊介绍:
Diagnostic Microbiology and Infectious Disease keeps you informed of the latest developments in clinical microbiology and the diagnosis and treatment of infectious diseases. Packed with rigorously peer-reviewed articles and studies in bacteriology, immunology, immunoserology, infectious diseases, mycology, parasitology, and virology, the journal examines new procedures, unusual cases, controversial issues, and important new literature. Diagnostic Microbiology and Infectious Disease distinguished independent editorial board, consisting of experts from many medical specialties, ensures you extensive and authoritative coverage.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


