抗生素耐药性和克雷伯氏菌在人类、动物和食物来源中的新序列类型:来自尼日利亚北部的同一健康观点
IF 5.8
Q1 MICROBIOLOGY
引用次数: 0
摘要
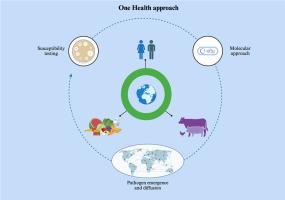
本研究旨在评估来自人类、动物和食物来源的克雷伯氏菌的基因组特征,并建立其与全球流行序列类型(STs)的克隆关系。采用表型和下一代测序方法,共收集和分析了300份样本,其中包括食品样本(n = 180)和人类临床样本(n = 120)。其中,从人(16)、动物(15)和食物(14)中分离出45株克雷伯氏菌。肺炎克雷伯菌为优势菌种(34/45,75.5%),其次为变异克雷伯菌亚种。variicola(4/45; 8.8%),准肺炎克雷伯菌(3/45;6.6%),肺炎克雷伯菌亚种。类似肺炎菌(2/45;4.4%)、产气克雷伯菌(1/45;2.2%)和密歇根克雷伯菌(1/45;2.2%)。综合所有来源,对甲氧苄啶-磺胺甲恶唑的耐药率为57.8%,对氨曲南(17.8%)、头孢多肟(17.8%)、头孢噻肟(22.2%)、头孢他啶(22.2%)、环丙沙星(24.4%)、粘菌素(15.6%)、庆大霉素(8.9%)、左氧氟沙星(2.2%)和妥布霉素(11.1%)的耐药率较低。一般来说,在人类和动物来源的样本中检测到耐药菌株的频率高于在食品来源的样本中检测到耐药菌株的频率。共鉴定出17个不同的STs,其中9个为新STs。氟喹诺酮类药物耐药主要是由于qnrS1基因的存在(33%),而氨基糖苷类药物的耐药基因为strB(22%)、strA(17.7%)和aac(6′)-Ibr-cr(11.1%)。β-内酰胺耐药基因blaCTX−M、blaSHV、blaTEM、blaOXA和blaOKP-B在人(15/16;93.7%)和动物(17/19;89.5%)分离株中大量存在。在esbl编码基因中,blaOXY-1(1/10; 10%)只存在于食品样品中。克雷伯氏菌在人类、动物和食物生态位中具有相同STs的耐抗生素和新谱系的出现,表明高危菌株的克隆扩增。尼日利亚北部迫切需要使用“同一个健康”方法监测和控制产生esbl的肠杆菌科。本研究有助于了解尼日利亚克雷伯氏菌的流行病学。该研究强调,即使在最后使用抗生素相对有限的地区,高风险的全球克隆也在传播。这些发现与“同一个健康”方针一致,并强调了人类、动物和食物来源之间的密切联系,这促进了普通克隆的传播。鉴于克雷伯氏菌不断出现新的耐药机制,有必要在整个非洲采用经典方法和分子方法进行持续监测。在这项研究中,下一代测序能够对循环细菌种类、抗性组、质粒组和病毒组进行全面评估。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Antibiotic resistance and novel Sequence Types of Klebsiella spp. in human, animal, and food sources: a One Health perspective from Northern Nigeria
This study aimed to evaluate the genomic characteristics of Klebsiella spp. from human, animal, and food sources, and to establish their clonal relationships with globally circulating sequence types (STs). Using both phenotypic and next-generation sequencing approaches, a total of 300 samples comprising food samples (n = 180) and human clinical samples (n = 120) were collected and analyzed. Of these, 45 Klebsiella spp. were isolated from human (n = 16), animal (n = 15), and food (n = 14) sources. K. pneumoniae was the predominant species (34/45; 75.5%), followed by K. variicola subsp. variicola (4/45; 8.8%), K. quasipneumoniae (3/45; 6.6%), K. pneumoniae subsp. similipneumoniae (2/45; 4.4%), K. aerogenes (1/45; 2.2%), and K. michiganensis (1/45; 2.2%). Considering all the sources, 57.8 % of the isolates resulted in resistant to trimethoprim-sulfamethoxazole, while a lower percentage of strains showed resistance to aztreonam (17.8%), cefpodoxime (17.8%), cefotaxime (22.2%), ceftazidime (22.2%), ciprofloxacin (24.4%), colistin (15.6%), gentamicin (8.9%), levofloxacin (2.2%) and tobramycin (11.1%). In general, resistant strains were detected more frequently in samples of human and animal origin than in those of food origin. A total of 17 distinct STs were identified, including 9 novel STs. The fluoroquinolones resistance was mainly attributed to the presence of gene qnrS1 (33%), while strB (22%), strA (17.7%), and aac (6′)-Ibr-cr (11.1%) for aminoglycoside. β-lactam resistance genes blaCTX−M, blaSHV, blaTEM, blaOXA, and blaOKP-B were considerably present in human (15/16; 93.7%) and animal (17/19; 89.5%) isolates. Among ESBL-encoding genes, blaOXY-1 (1/10; 10%) was exclusively found in food samples. The emergence of antibiotic-resistant and novel lineages of Klebsiella spp., with identical STs across human, animal, and food niches, indicates clonal expansion of high-risk strains. Surveillance and control of ESBL-producing Enterobacteriaceae using the One Health approach are urgently needed in Northern Nigeria.
Importance
. This study contributes to the understanding of the epidemiology of Klebsiella spp. in Nigeria. The study highlights that even in regions with relatively limited use of last resort antibiotics, high-risk global clones are circulating. These findings, aligned with the One Health approach, and emphasize the close interconnection between human, animal, and food sources, which facilitates the spread of common clones. Given the continuous emergence of new resistance mechanisms in Klebsiella spp., ongoing surveillance across Africa is warranted, employing both classical and molecular methods. In this study, next-generation sequencing enabled a comprehensive assessment of the circulating bacterial species, resistome, plasmidome, and virulome.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Current Research in Microbial Sciences
Immunology and Microbiology-Immunology and Microbiology (miscellaneous)
CiteScore
7.90
自引率
0.00%
发文量
81
审稿时长
66 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


