早期时间窗内血管内血栓切除术前MRI与CT对比:一项系统回顾和荟萃分析
IF 3.3
3区 医学
Q2 CLINICAL NEUROLOGY
引用次数: 0
摘要
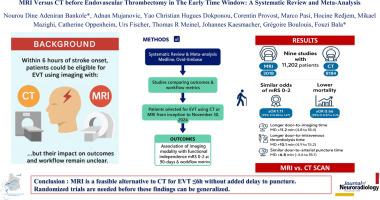
背景选择急性脑卒中患者在症状出现后6小时内进行血管内血栓切除术(EVT)可以通过MRI或CT进行。然而,成像方式与更好的临床结果或更短的工作流程时间之间的关系仍未完全了解。方法:我们检索Medline和ovd - embase,以比较从开始到2024年11月30日使用CT或MRI进行EVT的患者的结果和工作流程指标的研究。主要结果是成像方式与90天功能独立性(修改Rankin量表评分,0-2)和工作流程指标的关联。采用随机效应模型计算95% ci的合并优势比。结果9项研究共纳入11202例患者(MRI 3018例,CT 8184例)。与选择CT的患者相比,选择MRI的患者90天mr0 - 2的比值相似(校正比值比[aOR] 1.1195% CI 0.84-1.47),死亡率更低(aOR 0.6695% CI 0.57-0.76)。在选择MRI的患者中,门到成像时间(平均差[MD] 11.2分钟,95% CI 4.8至18.4)和门到静脉溶栓起始时间(MD 10.1分钟,95% CI 4.9至15.2)更长。然而,两组之间的门到动脉穿刺时间相似(MD 6.8 min, 95% CI -4.6至18.1)。结论对于症状出现后6小时内行EVT的脑卒中患者,EVT前MRI检查可替代CT检查,且从开门到穿刺时间无明显延迟。在这些发现可以推广之前,需要进行随机试验。本文章由计算机程序翻译,如有差异,请以英文原文为准。
MRI versus CT before endovascular thrombectomy in the early time window: A systematic review and meta-analysis
Background
Selection of acute stroke patients for endovascular thrombectomy (EVT) within 6 h from symptom onset can be done using MRI or CT. However, association of either imaging modality with better clinical outcomes or shorter workflow times is still not fully understood.
Methods
We searched Medline and Ovid-Embase for studies comparing outcomes and workflow metrics between patients selected for EVT using CT or MRI from inception to November 30, 2024. The primary outcome was the association of imaging modality with functional independence (modified Rankin Scale score, 0–2) at 90-days and workflow metrics. Pooled odds ratios with 95% CIs were calculated using a random-effects model.
Results
Nine studies with 11,202 patients (3018 with MRI vs 8184 with CT) were analysed. Patients selected with MRI had similar odds of 90-day mRS 0–2 (adjusted odds ratio [aOR] 1.1195% CI 0.84–1.47) and lower mortality (aOR 0.6695% CI 0.57–0.76) compared to those selected with CT. Door-to-imaging time (mean difference [MD] 11.2 min 95% CI 4.8 to 18.4) and door-to-intravenous thrombolysis initiation time (MD 10.1 min 95% CI 4.9 to 15.2) were longer in patients selected with MRI. However, door-to-arterial puncture time was similar between both groups (MD 6.8 min 95% CI -4.6 to 18.1).
Conclusion
In stroke patients undergoing EVT within 6 h from symptom onset, MRI before EVT could be a feasible alternative to CT without significant delays from door to puncture time. Randomized trials are needed before these findings can be generalized.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Journal of Neuroradiology
医学-核医学
CiteScore
6.10
自引率
5.70%
发文量
142
审稿时长
6-12 weeks
期刊介绍:
The Journal of Neuroradiology is a peer-reviewed journal, publishing worldwide clinical and basic research in the field of diagnostic and Interventional neuroradiology, translational and molecular neuroimaging, and artificial intelligence in neuroradiology.
The Journal of Neuroradiology considers for publication articles, reviews, technical notes and letters to the editors (correspondence section), provided that the methodology and scientific content are of high quality, and that the results will have substantial clinical impact and/or physiological importance.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


