退行性颈椎病患者后路减压术后不良预后的预测因素。
IF 2.2
4区 医学
Q3 CLINICAL NEUROLOGY
引用次数: 0
摘要
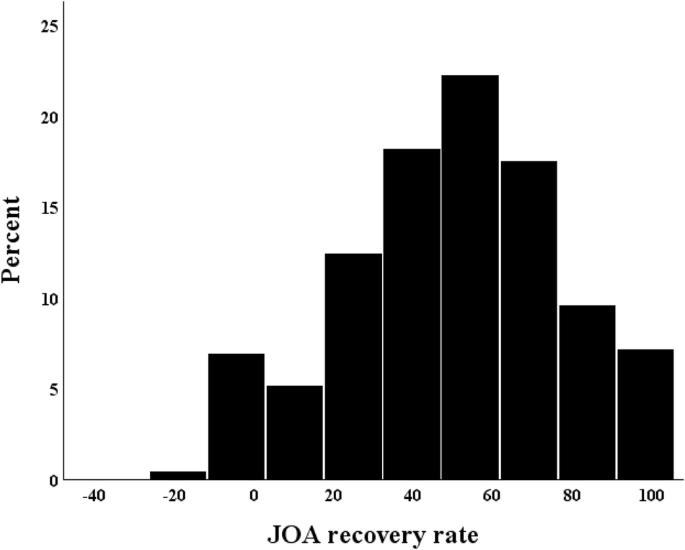
研究设计:回顾性多中心研究。目的:确定与退行性颈椎病(DCM)后路减压术后神经系统改善失败相关的预测因素。背景:日本17所院校。方法:采用后路减压术,随访10年。测定日本骨科协会(JOA)的康复率,并根据JOA康复率将患者分为3个结局组:公平组(康复率77.2%:平均+1 SD)。评估人口统计信息、术后并发症和影像学参数,并使用多项逻辑回归分析确定不良预后的预测因素。结果:纳入的868例患者中,一般组140例(16.1%),中等组586例(67.5%),良好组142例(16.3%),平均JOA恢复率分别为6.2%±13.7%,50.1%±15.0%和90.6%±8.3%。虽然在单因素分析中,三组患者的糖尿病发生率有显著差异(26.4% vs. 23.0% vs. 14.1%, p = 0.03),但多项回归分析显示,在公平组和良好组的比较中,年龄是不良预后的显著独立预测因子(优势比[OR], 1.62; 95%可信区间[CI], 1.27-2.07;结论:年龄可能是DCM患者后路减压术后神经系统改善失败的独立预测因素。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Predictors of poor outcomes after posterior decompression surgery in patients with degenerative cervical myelopathy
Retrospective multicenter study. To identify predictors associated with failure of neurological improvement after posterior decompression surgery for degenerative cervical myelopathy (DCM). 17 institutions in Japan. Patients who underwent posterior decompression surgery and were followed up for >1 year were enrolled. The Japanese Orthopedic Association (JOA) recovery rate was determined, and patients were divided into three outcome groups based on the JOA recovery rate: fair (recovery rate, <22.2%: mean-1SD), moderate (22.3%–77.1%), and good (>77.2%: mean+1 SD) groups. Demographic information, postoperative complications, and radiographic parameters were assessed, and predictors of poor outcomes were identified using the multinominal logistic regression analysis. Of 868 patients enrolled, 140 (16.1%), 586 (67.5%), and 142 (16.3%) were assigned to the fair, moderate, and good groups, respectively, with mean JOA recovery rates of 6.2% ± 13.7%, 50.1% ± 15.0%, and 90.6% ± 8.3%. Although there were significant differences in the frequency of diabetes mellitus among the three groups in the univariate analysis (26.4% vs. 23.0% vs. 14.1%; p = 0.03), the multinominal regression analysis revealed that old age was a significant independent predictor of poor outcomes in the comparison between the fair and good groups (odds ratio [OR], 1.62; 95% confidence interval [CI], 1.27–2.07; p < 0.01). Old age was also significantly associated with failure of neurological improvement between the fair and moderate groups (OR, 1.35; 95% CI 1.15–1.59; p < 0.01). Old age may be an independent predictor of failure of neurological improvement after posterior decompression surgery in patients with DCM.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Spinal cord
医学-临床神经学
CiteScore
4.50
自引率
9.10%
发文量
142
审稿时长
2 months
期刊介绍:
Spinal Cord is a specialised, international journal that has been publishing spinal cord related manuscripts since 1963. It appears monthly, online and in print, and accepts contributions on spinal cord anatomy, physiology, management of injury and disease, and the quality of life and life circumstances of people with a spinal cord injury. Spinal Cord is multi-disciplinary and publishes contributions across the entire spectrum of research ranging from basic science to applied clinical research. It focuses on high quality original research, systematic reviews and narrative reviews.
Spinal Cord''s sister journal Spinal Cord Series and Cases: Clinical Management in Spinal Cord Disorders publishes high quality case reports, small case series, pilot and retrospective studies perspectives, Pulse survey articles, Point-couterpoint articles, correspondences and book reviews. It specialises in material that addresses all aspects of life for persons with spinal cord injuries or disorders. For more information, please see the aims and scope of Spinal Cord Series and Cases.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


