减肥手术对高血压预后的影响:一项回顾性队列研究。
IF 3.4
4区 医学
Q2 PERIPHERAL VASCULAR DISEASE
引用次数: 0
摘要
代谢和减肥手术(MBS)是治疗肥胖和代谢综合征的有效方法。关于MBS对高血压预后影响的证据受到短期随访的限制。因此,本回顾性队列研究旨在比较接受和不接受MBS治疗的患者之间的血压(BP)控制、抗高血压药物(AHMs)数量、明显难治性高血压(ATRH)的发展以及高血压缓解情况。纳入了2000-2019年在退伍军人健康管理系统内接受治疗的BMI≥35 kg/m2和新诊断为高血压的成年人。使用广义估计方程和时间更新的Cox模型与逆概率处理权重来处理时间更新的混淆。在中位5.1年的随访中,183702例BMI≥35 kg/m2的高血压患者接受了医学治疗,3965例接受了手术治疗。基线时,接受MBS的患者中女性多于男性(22%对10%)。随着时间的推移,手术治疗的患者表现出明显更好的血压控制,平均收缩压降低5.4 mm Hg (95% CI 4.9-5.9),舒张压降低1.8 mm Hg (95% CI 1.5-2.1)。与接受药物治疗的患者相比,接受MBS的患者完全停止AHM的可能性高出32% (95% CI 1.23-1.42)。接受MBS治疗的患者发生ATRH的可能性降低14% (95% CI 0.78-0.95)。总体而言,在肥胖和高血压患者中,与医疗管理相比,MBS治疗与持续改善的血压控制相关,包括更低的收缩压和舒张压,更高的AHM终止率和更低的ATRH率。本文章由计算机程序翻译,如有差异,请以英文原文为准。
The Effect of Bariatric Surgery on Hypertension Outcomes: A Retrospective Cohort Study
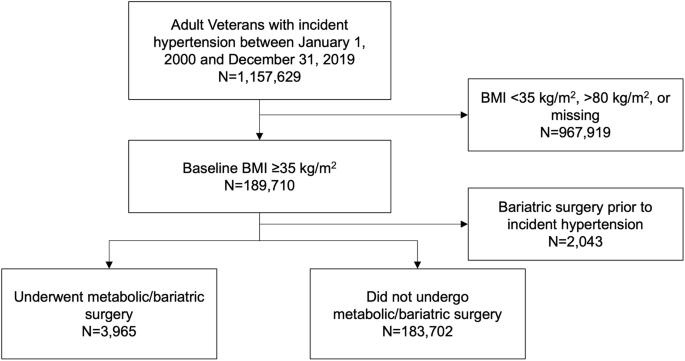
Metabolic and bariatric surgery (MBS) is an effective treatment for obesity and metabolic syndrome. Evidence regarding the impact of MBS on hypertension outcomes is limited by short-term follow-up. Thus, this retrospective cohort study was designed to compare blood pressure (BP) control, number of antihypertensive medications (AHMs), development of apparent treatment resistant hypertension (ATRH), and remission of hypertension between patients treated with and without MBS. Adults with BMI ≥ 35 kg/m2 and a new diagnosis of hypertension receiving care within the Veterans Health Administration system from 2000–2019 were included. Generalized estimating equations and time-updated Cox models with inverse probability of treatment weighting to address time-updated confounding were used. Over a median follow-up of 5.1 years, 183702 patients with BMI ≥ 35 kg/m2 and hypertension were managed medically and 3965 were managed surgically. At baseline, those who underwent MBS were more likely to be women than men (22 vs. 10%). Patients treated surgically demonstrated significantly better BP control over time, with an average 5.4 mm Hg (95% CI 4.9–5.9) lower systolic BP and 1.8 mm Hg (95% CI 1.5–2.1) lower diastolic BP. Compared to patients treated medically, those who received MBS had 32% higher likelihood of complete AHM discontinuation (95% CI 1.23–1.42). Patients treated with MBS were 14% less likely to develop ATRH (95% CI 0.78–0.95). Overall, among patients with obesity and hypertension, treatment with MBS was associated with durably improved BP control compared to medical management, including lower systolic and diastolic BPs, higher AHM cessation, and lower rates of ATRH.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Journal of Human Hypertension
医学-外周血管病
CiteScore
5.20
自引率
3.70%
发文量
126
审稿时长
6-12 weeks
期刊介绍:
Journal of Human Hypertension is published monthly and is of interest to health care professionals who deal with hypertension (specialists, internists, primary care physicians) and public health workers. We believe that our patients benefit from robust scientific data that are based on well conducted clinical trials. We also believe that basic sciences are the foundations on which we build our knowledge of clinical conditions and their management. Towards this end, although we are primarily a clinical based journal, we also welcome suitable basic sciences studies that promote our understanding of human hypertension.
The journal aims to perform the dual role of increasing knowledge in the field of high blood pressure as well as improving the standard of care of patients. The editors will consider for publication all suitable papers dealing directly or indirectly with clinical aspects of hypertension, including but not limited to epidemiology, pathophysiology, therapeutics and basic sciences involving human subjects or tissues. We also consider papers from all specialties such as ophthalmology, cardiology, nephrology, obstetrics and stroke medicine that deal with the various aspects of hypertension and its complications.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


