查加斯病心力衰竭患者的临床和流行病学特征:来自SEPE-HF登记的见解
IF 2.1
3区 医学
Q2 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
摘要
恰加斯心肌病(Chagas cardiomyopathy, Ch-CMP)是一种独特的心衰(HF)表型,在流行地区尚未得到充分研究,与非恰加斯心肌病相比,具有独特的临床、心电图和治疗特征。在巴西某三级中心417例因失代偿性心衰住院的患者中,155例(37.1%)确诊为Ch-CMP。Chagas患者年龄较小(平均年龄67.5 vs 67.7岁,p = 0.86),BMI较低(28.65 vs 25.40, p < 0.001),男性比例较高(50.9% vs 47.7%, p = 0.56)。Chagas组的合并症发生率较低,包括高血压(49.6% vs 70.1%, p = 0.001)和缺血性心脏病(3.2% vs 16.6%, p = 0.001)。Chagas患者的心电图异常更为普遍,如右束支传导阻滞(17.6% vs 9%, p = 0.015)、心房颤动(37.9% vs 23%, p = 0.001)和起搏器节律(22.2% vs 3.7%, p = 0.001)。收缩功能障碍(LVEF < 40%)在查加斯更为常见(59.4% vs 27.1%, p = 0.001)。尽管存在这些差异,但心血管住院死亡率没有显著差异(8.4% vs 5.2%, p = 0.279)。两组患者在出院时使用指南指导的药物治疗都不理想,但在查加斯患者中甚至更低,特别是β受体阻滞剂(52% vs 64%, p = 0.02)和ACEi/ARB/ARNi (54% vs 68%, p = 0.01)。整个队列中只有64%的患者使用循环利尿剂;在不需要利尿剂的患者中,心律失常和感染是入院的主要原因,房颤22例,感染21例。总之,恰加斯心肌病仍然是流行地区HF住院的主要原因,具有独特的心律失常和血管舒张特征,传统危险因素的患病率较低,出院时的治疗差距值得有针对性的干预。本文章由计算机程序翻译,如有差异,请以英文原文为准。
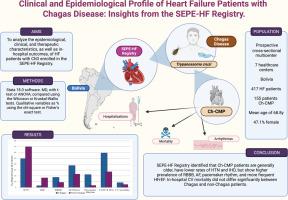
Clinical and Epidemiological Profile of Heart Failure Patients With Chagas Disease: Insights From the SEPE-HF Registry
Chagas cardiomyopathy (Ch-CMP) represents a unique and understudied phenotype of heart failure (HF) in endemic regions, with distinct clinical, electrocardiographic, and therapeutic characteristics compared to non-Chagas HF. In this retrospective cohort of 417 patients hospitalized for decompensated HF at a tertiary center in Brazil, 155 (37.1%) had confirmed Ch-CMP. Chagas patients were younger (mean age 67.5 vs 67.7 years, p = 0.86), had lower BMI (28.65 vs 25.40, p < 0.001), and a higher proportion of males (50.9% vs 47.7%, p = 0.56). Comorbidities were less frequent in the Chagas group, including hypertension (49.6% vs 70.1%, p = 0.001) and ischemic heart disease (3.2% vs 16.6%, p = 0.001). Electrocardiographic abnormalities were more prevalent among Chagas patients, such as right bundle branch block (17.6% vs 9%, p = 0.015), atrial fibrillation (37.9% vs 23%, p = 0.001), and pacemaker rhythms (22.2% vs 3.7%, p = 0.001). Systolic dysfunction (LVEF < 40%) was more common in Chagas (59.4% vs 27.1%, p = 0.001). Despite these differences, cardiovascular inhospital mortality did not significantly differ (8.4% vs 5.2%, p = 0.279). The use of guideline-directed medical therapy at discharge was suboptimal in both groups, but even lower in Chagas patients, particularly for beta-blockers (52% vs 64%, p = 0.02) and ACEi/ARB/ARNi (54% vs 68%, p = 0.01). Loop diuretics were used in only 64% of the entire cohort; among those not requiring diuretics, arrhythmias and infections were the leading causes of admission, atrial fibrillation in 22 patients, and infection in 21. In conclusion, Chagas cardiomyopathy remains a major contributor to HF hospitalizations in endemic regions, with a unique arrhythmogenic and vasodilated profile, lower prevalence of traditional risk factors, and concerning therapeutic gaps at discharge that merit targeted intervention.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

American Journal of Cardiology
医学-心血管系统
CiteScore
4.00
自引率
3.60%
发文量
698
审稿时长
33 days
期刊介绍:
Published 24 times a year, The American Journal of Cardiology® is an independent journal designed for cardiovascular disease specialists and internists with a subspecialty in cardiology throughout the world. AJC is an independent, scientific, peer-reviewed journal of original articles that focus on the practical, clinical approach to the diagnosis and treatment of cardiovascular disease. AJC has one of the fastest acceptance to publication times in Cardiology. Features report on systemic hypertension, methodology, drugs, pacing, arrhythmia, preventive cardiology, congestive heart failure, valvular heart disease, congenital heart disease, and cardiomyopathy. Also included are editorials, readers'' comments, and symposia.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


